Table of contents
DEFINE
Fibrous dysplasia of bone is a chronic, benign, non-hereditary bone disease in which normal bone is replaced by fibrous tissue. It is a scar-like lesion (fibrous tissue) that develops in normal bone.
Fibrous dysplasia is a rare bone disease that accounts for about 5% bone tumor benign, sporadic appearance.
The disease usually occurs in adolescence, between the ages of 3 and 15. Most people have symptoms before the age of 30. The ratio of men and women is about equal.
Clinical features of the disease are benign progressive bone lesions, bone deformities, bone pain, fracture.
CAUSE, PATIENTS
Fibroblastic dysplasia is the result of a random mutation in the GNAS gene at chromosomes 20q13.2 – q13.3 (encoding for the α subunit of the Gs-coupled protein receptor) of osteoblasts. In bone, constitutive Gsα signals lead to the differentiation and proliferation of osteoblasts. These poorly differentiated osteoblasts also increase interleukin IL-6 production, which increases the activity of osteoclasts, causing osteolytic lesions in the form of cavities in fibrous tissue as well as in surrounding healthy bone. . One or more areas of bone that are not normally mature and remain in a trabecular, poorly mineralized abnormal arrangement, scattered in dysplastic fibrous tissue. As bone grows, soft fibrous tissue spreads, weakening, deforming, and breaking easily.
The term fibrous dysplasia is Lichtenstein Named in 1938. One or more regions of bone that did not mature normally and remained in the form of a trabecular, poorly mineralized, irregularly arranged, scattered in dysplastic fibrous tissue. As bone grows, soft fibrous tissue spreads, weakening, deforming, and breaking easily.
The bone marrow stromal cells in fibrous dysplasia produce excess amounts of phosphate-regulating hormone growth factor-23 (FGF23), which leads to loss of phosphate in the urine. Patients with hypophosphataemia may develop rickets, osteomalacia, and bone pain.
DIAGNOSE
Implementing the quadrants
Mainly based on clinical and imaging studies, especially imaging X-ray featured.
1. Clinical
The clinical manifestations are diverse, ranging from a solitary, asymptomatic lesion discovered incidentally, to severe disability involving the entire skeleton and leading to loss of vision and hearing. sense and/or locomotion.
Skeletal dysplasia can occur in many bones or only in one bone, so there are different clinical manifestations:
- Symptoms in bones:
Bone pain, usually mild to moderate dull ache
+ Swollen
+ Bone deformity
+ Pathological fractures, especially in the arms and legs (Figure 34.1)
+ Difficulty walking, crooked leg bones
+ Rickets
+ Complications of bone cancer (bone sarcoma, fibrosarcoma, chondrosarcoma).
Commonly affected bones: femur, tibia, humerus, skull, ribs, pelvis, etc.
![Fibrous Dysplasia 1 Loạn Sản Xơ Xương ở Xương đùi. Phim X-quang Cho Thấy Gãy Xương ở Vị Trí đỉnh Mũi Tên [1]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Loan-san-xo-xuong-o-xuong-dui.-Phim-X-quang-cho-thay-gay-xuong-o-vi-tri-dinh-mui-ten-1-220x300.png)

(c) X-ray showing destruction of the maxillary bone, (d) View from the oral cavity – The amount of bone removed, (e) X-ray of the skull after surgery, (f) Postoperative image. Source: Cranial fibrous dysplasia: Surgery and literature review – Original article – practice guidelines (2013)
+ Extraskeletal lesions: in rare cases, fibrotic dysplasia may be associated with endocrine abnormalities (precocious puberty, hyperthyroidism, hyperparathyroidism, Cushing's syndrome, pituitary lesions), chromatic plaques skin factor. Increased bone pain may also be related to the normal hormonal changes of the menstrual cycle or pregnancy.
2. Subclinical
- X-ray: intramedullary damage to the bone body makes the bone transparent, has a blurred glass image, with thin cortical bone, deformed flexion of the bone; transparent lesions with thick fibrous margins, called the bark sign; cystic lesions: radiolucent with reactive border, no trabecular, cortical thickness is still normal; Paget's lesion type: trabeculae are denser than normal; shepherd's stick deformity: progressive lesion on the femur, causing a shepherd's club-like inward curvature. Transparent, fibrous lesions, solitary or multifocal, with or without asymmetry, may be seen on the craniofacial bone. The radiographic feature of malignancy is either a rapid increase in the size of the lesion or a change in mineralization of the bone by the resorption of the lesion.

lumbar and left femur [4]
CT-scan: evaluate the progression of bone lesions, especially in complex locations such as the spine, pelvis, rib cage or craniofacial bone, as well as the spread of the lesion to the paraspinal soft tissue.
- Nuclear magnetic resonance: assess the progression of the lesion, the possibility of pathological fracture, the possibility of malignancy of the bone lesion, or assess the spinal cord compression when the spine is injured. Gadolinium-injected MRI can also assess postoperative recurrence.
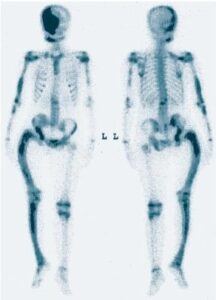
- T-99 bone scintigraphy: increased radioactivity in advanced lesions, helping to identify asymptomatic lesions (Figure 34.4). However, the lesion picture is not specific.
IMAGE
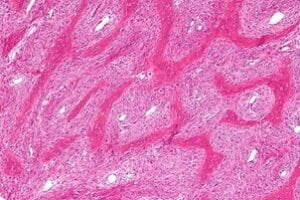
- Histopathological examination: a needle biopsy may be used to confirm the diagnosis. Macroscopically, a osteosarcoma is a solid white, or dark, mass. Microscopically, pathological bone consists of a mixture of immature fibrous tissue and immature trabecular fragments. The trabeculae are thin, irregular, shaped like Chinese letters (Figure 5).
Blood tests: increased levels of alkaline phosphatase. Urinalysis showed increased hydroxyproline levels. However, these abnormalities are not specific for fibrous dysplasia.
Diagnosis of disease
– One drive: most patients have only one bone (70% cases)
The disease is usually found in adults, between the ages of 20 and 30. Lesions may be asymptomatic, or local bone pain, or fracture easily. The most commonly injured bones are the ribs, skull, face, especially the jawbone, the metaphysis or the bony body of the upper head of the femur or tibia. Most (95%) disease self-resolved after adulthood, lesions do not grow anymore.
– Multi-drive form ( 30% case )
The disease is more severe with multiple and widespread lesions, causing many symptoms and complications. The disease is usually detected as early as 10 years old. Usually one side of the body is affected. However, about a quarter of patients with polymorphic lesions have more than half of the skeleton, especially in the lower extremities. Injury to the facial bones of the skull is seen in 1/2 patients with multiple bone lesions. When the skull is damaged, the patient's face may have symptoms of nerve vascular compression such as headache, tinnitus, loss of vision, cranial nerve abnormalities, even spontaneous brain bleeding. Temporal bone dysplasia, which often affects the auditory canal with possible hearing loss and occlusion of the external ear, is more common in patients with McCune-Albright syndrome associated with growth hormone excess.
The multifocal form can be associated with precocious puberty, fibrous dysplasia, and milky-coffee-colored skin, called Albright syndrome or mucinous striated muscle tumor (Mazabraud syndrome).
Fibrous dysplasia usually involves the spine, which can lead to scoliosis, which in rare cases can be severe. Left untreated, progressive scoliosis is one of the few features of fibrous dysplasia that can lead to early death.
Prognosis: monofocal has a good prognosis. Multifocal lesions tend to get worse, sometimes they can become malignant into osteosarcoma or fibrosarcoma.
Differential diagnosis
- Hyperparathyroidism
- Neurofibromatosis
TREATMENT
General principles
There is no specific treatment to cure the disease. Asymptomatic patients do not need treatment, only monitoring. There is almost no treatment for skin lesions or precocious puberty. Treatment is usually aimed at addressing the bone lesions and depending on the type of disease one or more bones. Radiation therapy is contraindicated because it can transform into osteosarcoma. Chemotherapy did not work.
Treatment includes conservative and surgical measures, depending on the location and extent of bone damage. Patients need to be followed up every 6 months, clinical examination, laboratory tests and X-rays to detect complications of the disease such as optic nerve compression.
Specific treatment
- Internally medical treatment:
Bone pain relief:
Common pain relievers. Drug use according to the World Health Organization ladder. Choose one of the following drugs:
- Paracetamol 0.5 g × 2 – 4 tablets/24 hours.
- Paracetamol combined with codeine or tramadol: 2-4 tablets/24 hours. Non-steroidal anti-inflammatory drugs appoint one of the following drugs:
- Diclofenac 50 mg × 2 tablets/day, piroxicam 20 mg × 1 tablet/day, meloxicam 7.5 mg × 1-2 tablets/day, celecoxib 200 mg × 1-2 tablets/day
- Etoricoxib tablets 30 mg, 60 mg × 1 tablet/day
Bisphosphonates can be used to relieve chronic bone pain, increase bone density in the spine and femur, and reduce the risk of fractures:
- Alendronate 70 mg x 1 tablet/week for 3 years.
- Pamidronate 60 mg, IV phase 60 mg/day, for 3 consecutive days and repeated after 6 months, for a minimum of 2 years. Re-treatment is possible after 1 year, depending on clinical response to analgesia, biological tests or radiographs.
- Zoledronic acid 5 mg × IV phase once a year for a minimum of 2 years, then can be re-treated after 1 year.
Calcium and vitamin D supplementation during bisphosphonate therapy to avoid secondary hyperparathyroidism:
- Vitamin D3 × 800 UI/day, calcium 500 - 000 mg/day. Add phosphorus when there is a deficiency.
Calcitonin is only effective in multifocal form with bone pain and elevated alkaline phosphatase:
- Calcitonin tube 50 UI, 100 UI, intramuscular injection 50-100 UI/day.
Quản lý nội tiết là một thành phần quan trọng của quản lý trong loạn sản xương. Tất cả bệnh nhân mắc chứng loạn sản sợi nên được đánh giá và điều trị các bệnh nội tiết liên quan đến hội chứng McCune-Albright. Đặc biệt, sự dư thừa hormone tăng trưởng không được điều trị có thể làm trầm trọng thêm chứng loạn sản xơ xương sọ và làm tăng nguy cơ mù lòa. Điều trị các rối loạn nội tiết như: hội chứng cường giáp trạng, hội chứng Cushing, đái tháo đường, dậy thì sớm kèm theo bằng các thuốc thích hợp hay phẫu thuật nếu có chỉ định.
- Surgical treatment:
The goal of surgical treatment is to prevent and treat severe bone deformities and fractures, especially load-bearing bones; overcome the difference in lower limb length; release nerve compression, especially in the craniofacial region. Treatment works to straighten and strengthen damaged bones.
- Indications for surgical treatment: failure of conservative treatment; displaced, non-healing fractures; frequent pain; progressive deformity; oncology; Prevents extensive damage that can lead to fractures.
- Surgery depends on the location of the damaged bone, including dredging the lesion, fusion surgery, autologous or allogeneic bone grafting, orthopedic and fixed with nails, screws. The recurrence rate is high after curettage and bone grafting, especially in pediatric patients. Bone resection and curettage are not indicated when dysplasia recurs. Progressive scoliosis can generally be managed with standard instrumentation and fusion techniques. Surgical management of the cranium is complicated by frequent recurrences of fibrous dysplasia after surgery and should focus on correcting functional deformities.
PROGRESS AND COMPLAINTS
- Pathological fractures
- Malignancy of fibrous dysplastic lesions can occur, although rarely, with an incidence ranging from 0.5 to 3%. Malignancy usually occurs in polyostosis, usually in adulthood in lesions that have progressed for more than 13 years and reactivated multiple times (bone destruction, pain, fractures, etc.).
- Complications of nerve or vascular compression of bone lesions are headache, tinnitus, cranial nerve abnormalities, hearing loss, stenosis of the outer ear canal, spontaneous cranial bleeding when the skull is injured. Temporomandibular dysplasia can cause hearing loss and occlusion of the external ear cavity, asymmetry of the face, and protrusion of the eyes. Fractures occur with a high rate, in over 85% patients. Shortness occurs due to premature ossification of the bone head.
PREVENTION
Patients need to wear a brace to prevent fractures. Have a reasonable exercise regimen. Avoid carrying and doing heavy work. Fall prevention. It is necessary to periodically re-examine after 1-3 months, depending on the condition of the disease.



