Table of contents [hide]
OUTLINE
Pelvic (Pelvis) consists of two pelvises, at the back connected to the sacrum by two sacroiliac joints; anteriorly by the pubic joint. Each pelvis has a acetabulum which is a major component of the hip joint.
The pelvis is mostly spongy bone. In the pelvis there are weak areas such as the middle of the pelvis, the pubic branches and at the orifice of the sacrum.
The pelvis has many muscles that cover and a system of very strong ligaments that are responsible for holding the pelvis, protecting the internal organs and being the fulcrum of the lower extremities.

Figure 7.1. Anterior and posterior ligaments of the sacroiliac joint keep the pelvis stable (according to Rockwood & Green)
Injuries that break the pelvis are usually very strong injuries, so in addition to broken bones, attention must be paid to the combined injuries: abdomen, chest, urinary tract, genitals. Pelvic fractures, especially pelvic fractures, cause a lot of bleeding, so they are prone to complications from blood loss shock, sometimes death.
The treatment fracture Pots are not just for making bone healing but also requires restoration of anatomical shape: no narrowing of the pelvis, no narrowing and deviation of the bladder neck, no shortening of limbs, no sequelae of hip damage.
Unstable pelvic fractures will cause the patient a lot of pain when turning, so there is a high risk of complications from lying for a long time such as positional ulcers, urinary tract infections, pneumonia, etc.
Fractures of the pubic branch are often associated with damage to the bladder and urethra; The treatment must combine many departments: Orthopedics, Urology. Sometimes accompanied by rectal lesions, a temporary anal opening is required. Therefore, the care of a patient with a severe pelvic fracture will be extremely complex.
CLASSIFY
There are many classifications, but the simplest (according to Merle d'Aubigné) is divided into three main groups:
- Partial pelvic fracture: incomplete fracture of the pelvis, the pelvis is still stable.
- True pelvic fracture: makes the pelvis unstable.
- Pelvic fracture with acetabular rupture.
Partial fracture of the pelvis
These are pelvic lesions in one or two places above the pelvis without disrupting the pelvic girdle. The most common types of pelvic fractures are:
- Pelvic wing.
- Fracture 1 - 2 pubic branches or unilateral dorsum Mechanism is usually direct trauma.
Clinical symptoms
Broken pelvis
- Swelling on one side of the pelvis
- Pain when pressing on the pelvis; Pelvic squeezing is painful and crunching can be heard
- Anterior iliac spine on one side can be lowered
- Bilateral hip movement painless.
Broken 1-2 branches of pubic bone
- Swelling on one side of the pubic bone near the inguinal folds, possibly perineal bruising (butterfly bruising)
- Sharp pain (painful pelvic squeezing)
- Mobility of the hip joint usually causes less pain on the side of the fracture.
X-optical
X-rays are used to confirm the diagnosis.
Treatment
This type of pelvic fracture is stable, easy to heal, usually just let the patient rest in bed for a while, when the pain is gone, you can sit up and practice walking.
For hip fracture, if there is a lot of displacement; sometimes form a large hematoma. Broken bones can be straightened but difficult to keep, therefore, need to fix surgery with spongy visor or splint.
Good prognosis.
Complete pelvic fracture
Also known as true pelvic fracture; This type of fracture is severe and destabilizes the pelvis.
Classify
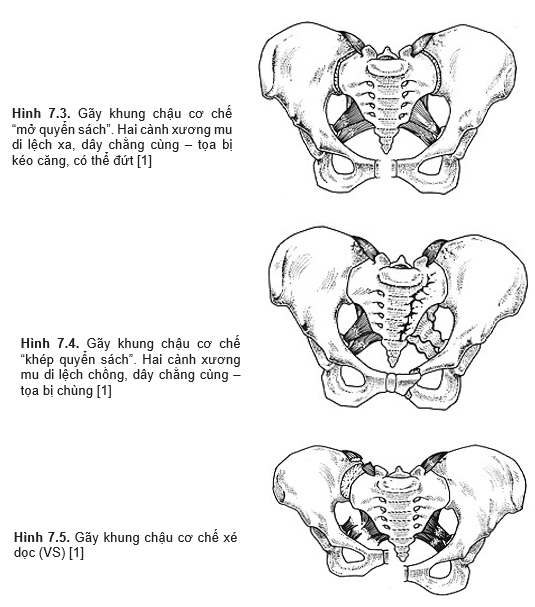
The Pennal and Tile classification of complete pelvic fractures has three main mechanisms. The anatomical damage depends on the mechanism of injury.
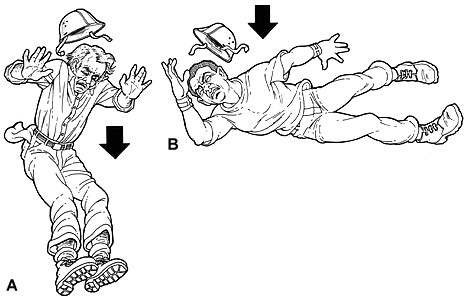
Figure 7.2. Mechanism of pelvic fracture injury: longitudinal tear force (A); lateral compression (B) [1]
- APC: (Antero-Posterior Compression): this mechanism is likened to "opening a book". Compressed force from front to back. For example, being pressed between two carriages, being directly hit by a car accident, being pressed by a wall, etc. If the pressure is right in the middle of the pubic joint, four pubic bones may be broken, and the bladder and urethra may be ruptured. . If the pressure is on one side of the iliac wing, it is possible to break the two pubic branches with distal displacement or dislocation of the pubic joint; sacroiliac joint with rupture of the anterior sacroiliac ligament.
- LC: (Lateral Compression): This mechanism is likened to "closing the book". Pressure from one side. Injury can be encountered: fracture of two branches of the pubic bone displaced superimposed, on the same side or on both sides. Sacroiliac dislocation due to rupture of posterior sacroiliac ligament. Injury to the Sacrospinous ligament and Sacrotuberous ligament.
- VS: (Vertical Shear): vertical tearing force. Usually due to a fall from a height, causing displacement of one side of the pelvis upward. Common injuries are: pubic joint dissection or bicuspid fracture of the pubic bone displaced upward; posterior iliac or sacral dislocation or sacral fracture (commonly called Malgaigne fracture).
Clinical symptoms
The patient has symptoms of pelvic fracture: painful pelvic compressions, perineal and pelvic ecchymosis.
Asymmetrical pelvis:
- Externally rotated thigh, dilated pubic joint (in APC mechanism)
- Internally rotated thigh, in mechanism (LC)
- Short limbs but measuring absolute length and relatively not short (VS mechanism). Mobility of the hip joint may be limited because of pain and pelvic instability.
In addition, it is necessary to look for additional symptoms of associated injuries or complications such as shock, damage to the urethra, bladder, and rectum.
X-ray
Take a shot X-ray The entire pelvis is in the plane of the parietal plane.
- Identify broken and displaced lines
- Identify pubic and sacroiliac joints
- In the mechanism of APC: the iliac wing on the affected side is enlarged. In the LC mechanism the opposite is true.
To clearly see the anterior part of the waist and pelvis, it is necessary to take the “Inlet” position (take the face plane but the beam is 45 degrees away).o from top to bottom). To see the back of the pelvis, take the “Outlet” position (face-to-face but 45 . angle)o bottom up).
Treatment
Prioritize treatment before complications and associated injuries.
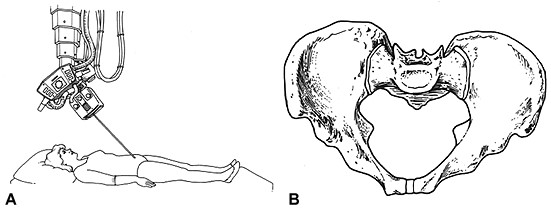
Figure 7.6. Pelvic X-ray “inlet” position A: shooting position; B: visible image [2]
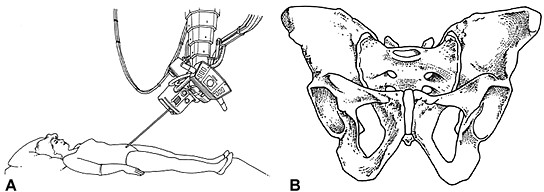
Figure 7.7. Pelvic X-ray “outlet” position A: shooting position; B: visible image [2]
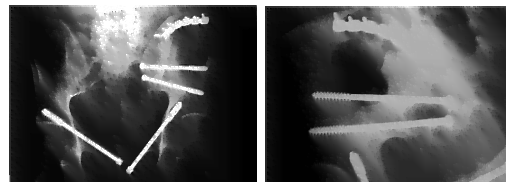
Figure 7.8. Treatment of pelvic fractures with bone fusion [3]
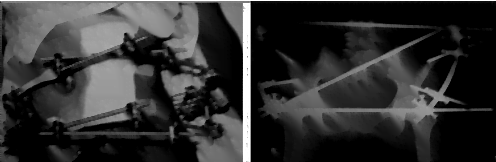
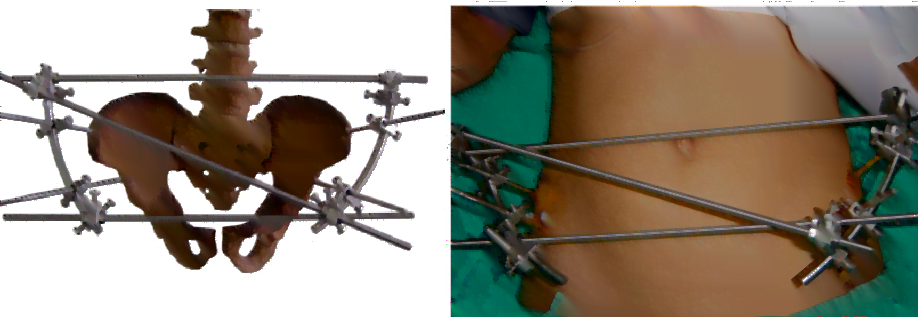
Figure 7.9. Treatment of pelvic fractures with external fixation [4]
Broken bones can be treated conservatively or surgically depending on the stability of the pelvis, accompanying injuries and complications. Specific treatments are:
- Bed rest for 2-4 weeks, Rotate to fight ulcers: applied to cases where the pelvis is still relatively stable, the bones move less, the patient does not have much pain when turning.
- Lying in a hammock: treatment of pubic joint dissection.
The hammock is made of thick, wide fabric that hugs the entire buttocks and hangs both ends up to the ceiling to raise the buttocks about 1-2 cm off the bed. Lying in a hammock to compress the pubic joint, keep it for 4-6 weeks for the ligaments to heal.
- Kéo liên tục qua lồi cầu xương đùi to pull down one side of the iliac wing in Malgaigne fracture (VS).
Set the external fixed frame
Gantz frame
Gantz frame: Use two large nails with a stopper at the top, place them behind the sides of the pelvis and then tighten them (thanks to the stopper at the top, the nail does not puncture the pelvis). The goal is to stop bleeding by compressing the fractured surfaces.
The advantage is that it is quick to place and does not cause problems when abdominal surgery is needed. Cons: the frame is not stable and does not fully correct the displacement.
Only use this frame in emergency to stop bleeding, prevent shock.
Rectangular frame
Use Schanz nails to place at least two nails on each side of the pelvis. Install the external fixing bracket securing the four nails like the four corners of a rectangle. The frame is adjustable, so it is possible to correct the bones so that the two fracture faces come together. The externally fixed pelvis will be more stable, helping the patient to turn easily and get up early.
The disadvantage of the frame is that it cannot be placed when there is a broken pelvis, causing entanglement in the abdomen, making it difficult to need an abdominal surgery, sometimes making it difficult for the patient to sit up. There can be infection of the nail and the correction is relative but not perfect, especially with VS fractures.
Combine bones
Used when external fixation is not satisfactory. Usually applied in sacroiliac dislocation and multiple pubic dislocations.
Symptoms
Pelvic fractures can have the following complications:
Early complications:
+ Traumatic shock: due to loss of blood and pain. Blood and fluid replacement is required, prophylactic pelvic anesthesia with 100-200 mL Novocain 0.25%
+ Bladder rupture: Intraperitoneal or extraperitoneal: urinary retention without bladder bridge, etc.
+ Posterior urethral rupture: urinary retention with bladder bridge + bleeding from the mouth and stoma...
+ Rectal perforation: rectal examination is required for diagnosis.
+ Pelvic vascular rupture: Resuscitation is active but blood pressure is still low and Hct is low, need exploratory surgery, if broken, it must be re-connected or tied if not the external iliac artery.
+ Open fracture: Note that all cases of urethral rupture and rectal perforation are considered open pelvic fractures.
- Late complications: deviation:
+ Narrowing the pelvic floor difficult to give birth
+ Narrowing of the bladder neck (due to displacement of pubic branches) makes it difficult for urethral surgery
+ Short legs walking for a long time deform the spine and damage the hip joints.
Fracture of the acetabulum
This is a type of penetrating fracture, which can cause the facet canal to increase, which can easily affect the hip joint function such as joint damage and stiffness.
Fracture of the acetabulum is also caused by a severe trauma, the mechanism can be direct (rolled over, crushed) or indirectly by strong impact of the femoral head.
Classify
The following fractures are commonly encountered:
- Pelvic wing fracture, pelvic waist violated the joint socket
- Fracture of the posterior margin of the acetabulum with posterior dislocation of the hip
- Fracture of many pieces of the acetabulum, the femoral head sinks inward, is called a central hip dislocation
According to Judet and Letournel, the pelvis is divided into two pillars:
+ Pubic or anterior iliac pillars
+ Seated or posterior iliac pillars. Depending on which pillar the fracture is located in, how it is displaced, there is a treatment direction. Judet – Letounel splits and breaks pan into two categories: simple and complex.
Simple fracture: Five styles:
- Broken back wall
- Rear pillar fracture
- Fracture of anterior wall
- Fracture of the front pillar
-
-
 Transverse fracture: fracture line from anterior to posterior abutment – alveolar arch where the weight is applied is intact.
Transverse fracture: fracture line from anterior to posterior abutment – alveolar arch where the weight is applied is intact.
-
-
Figure 7.10. Pelvic view externally and internally [1]
Complex fracture: There are also five styles
- TWO-shaped fracture
- Fracture of the posterior pillar combined with the posterior wall
- Horizontal fracture combined with posterior septum
- Fracture of the anterior septum or anterior pillar combined with transverse fracture of the posterior half
- Break both pillars.
Clinical symptoms:
- Swollen hip joint pain
- Pelvic squeezing pain
- Painful hip movement
- There may be external rotation or internal rotation distortion and short limbs
- There may be deformities such as dislocation of the hip (fracture of the posterior margin of the acetabulum with posterior dislocation of the hip).
X-ray
Straight pelvic imaging: view fracture lines and underlying displacements.
45 . internal rotation of the pelviso and rotated 45o Also known as Letournel pose to see the displacements of the front and rear pillars.
A CT-scan of the acetabulum is necessary to fully evaluate the displacement of the fracture fragments.
Treatment
- Non-displaced pelvic fracture: bed rest for 6-8 weeks, gentle hip exercise.
- Displaced pelvic fracture:
+ Posterior margin fracture + hip dislocation: nắn trật khớp, nếu sau khi nắn khớp tương đối vững tức là ít khả năng trật lại thì cast chậu bàn chân, trường hợp sau nắn khớp háng dễ dàng trật lại thí cần phải mổ đặt lại mảnh gãy và kết hợp xương bằng các vis xốp.
+ Multiple fractures displace the anterior posterior pillars:
- Continuous traction through the femoral condyle, after 2-3 days of x-ray examination, if there is a compatibility between the head and the acetabulum, maintain continuous traction for 6 weeks.
- In case the acetabulum is displaced a lot, there is a loss of compatibility between the crest and the acetabulum, it is necessary to have surgery to fuse the bones with a visor after reshaping the broken fragments.
Complications and consequences:
- Traumatic shock
- Misalignment → Easily damaged hip joint
- Dislocation or subdislocation of the hip.
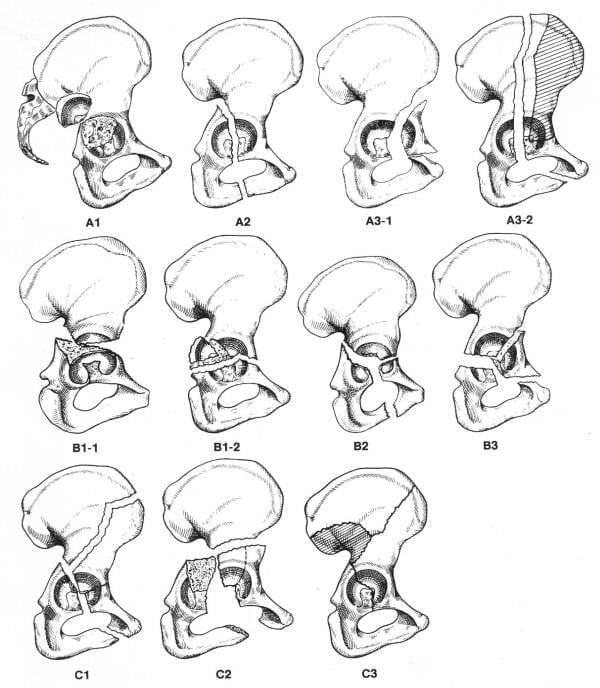
Figure 7.11. Classification of acetabular fractures according to A0
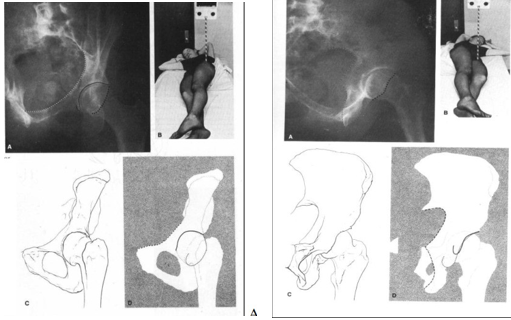
Figure 7.12. X-ray of the pelvis with internal or oblique rotation (A) and external or oblique rotation (B) (according to RockWood) [1]
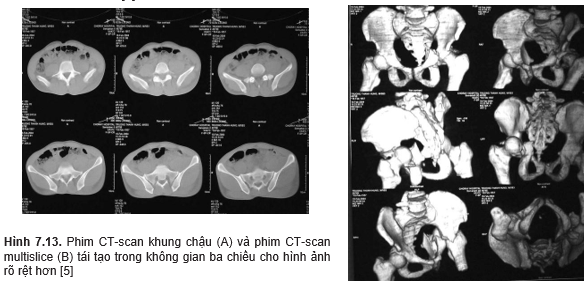
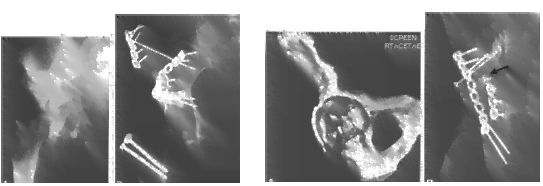
Figure 7.14. Complicated alveolar fractures with displacement of the facet joint are often treated surgically with osteosynthesis (according to Rockwood)




