FLOW MATCH
OUTLINE
Khuỷu là một khớp vững, nhưng trật khớp thường xảy ra và trật khớp tái hồi thì hiếm. Đây là loại trật khớp phổ biến nhất sau trật khớp vai và ngón tay.
Tỉ lệ mắc phải cao nhất ở tuổi 12 – 30 và thường liên quan đến sports injury.
Define
An elbow dislocation is when both ends of the ulnar and radial bones come out of the lower humerus. If the radial bone is in the normal position, an incomplete dislocation of the elbow or a dislocation of the radial head while the rotator cuff is trapped under the pulley is also considered an incomplete dislocation.
Anatomy
The elbow joint is the only joint consisting of three joints in a synovial space that covers the ligamentous joint: the ulnar humerus (elbow pulley), the radial humerus (external radial condyle) and the superior ulnar radial joint (little sigmoid fossa). rotating border).
The bony landmarks of the elbow process: the superior process of the lateral condyle, the apex of the pulley, the process of the elbow is palpable under the skin.
Biomechanics
- Morrey et al suggested that the useful (physiological) amplitude of the elbow joint:
- Flexing - stretching: 120° - 20°
- Pronation - supine forearm: evenly 50°.
- The stability of the elbow joint thanks to the static and dynamic stabilizers.
CLASSIFY
Classification is based on the relative position of the elbow to the humerus after injury. According to Howard SA can be classified as follows:
- Dislocation of both radial and ulnar bones: posterior, ulnar, radial, anterior, divergent (anteroposterior or bifurcated)
- Radial dislocation only: anterior, posterior, lateral
- Only ulnar dislocation: anterior, posterior.
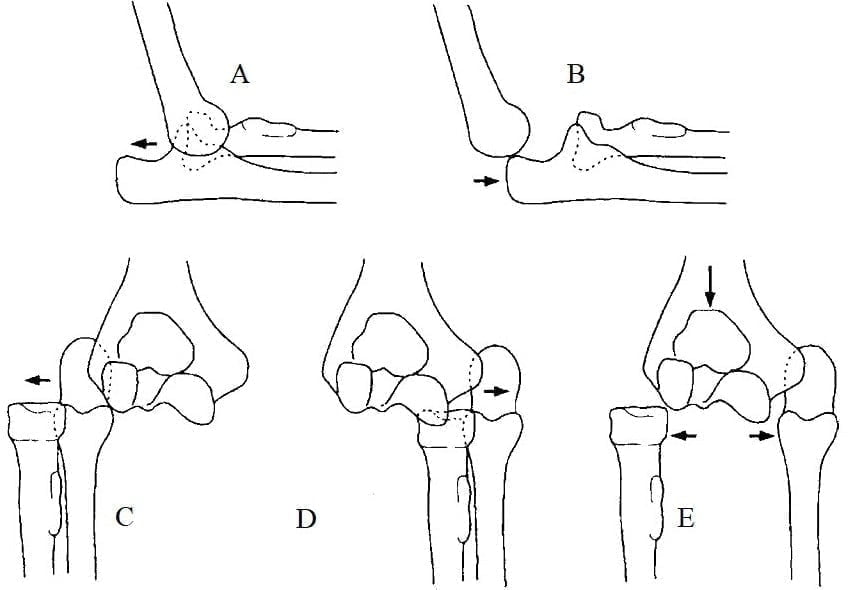
Figure 10.1. Classification of elbow dislocations
A. Back dislocation, B. Anterior dislocation, C. External dislocation, D. Inward dislocation, E. Divergent dislocation [1]
INJURY MECHANISM
- Often dislocated the elbow from falling on the hand or wrist while the forearm is extended and abducted.
- The most common site of elbow dislocation is overextension. When the force is transferred from the forearm (arms) to the elbow extension, the force in front pulls the ulna out of the pulley. As the joint continues to overextend, the anterior capsule and lateral ligament The outside is overstretched leading to the dislocation from the outside to the inside.
- The lateral curvature usually occurs when the forearm is prolapsed.
- Anterior dislocations are rare and are considered to affect the forearm posteriorly in mild flexion of the forearm, often with a fracture of the elbow.
- The anterior fascia of the medial collateral ligament is most important in stabilizing the posterior elbow.
DIAGNOSE
clinical
Specific symptoms
- Deformation:
- Elbow is slightly flexed 40 – 50°, cannot be straightened
- Side view: ax mark behind the elbow, the line drawn along the longitudinal axis of the humerus through the superior process of the lateral condyle without passing the elbow and radial head
- Palpation of the inferior humerus anterior to the elbow, changes in the landmarks of the triangle of Hueter (Nelaton, Malgaine).
- Spring sign (+)
- Signs of empty joint socket (+)
- Attention should be paid to neurovascular examination before and after manipulation because these two components are susceptible to damage during elbow dislocation and during elbow manipulation.
Subclinical
X-ray
- X-ray The classic upright and slanted posture is often sufficient to classify and evaluate associated lesions
- X-rays help identify dislocations and associated bone lesions.
Other laboratory tests
- MRI is useful in evaluating soft tissue injuries such as ligaments
- CT-scan helps to evaluate the degree of fracture of the radial head and condyle of the humerus in order to provide an appropriate method for open manipulation.
Acute complications
Blood vessel
- Early diagnosis of vascular injury is imperative
- When the pulse is lost, it is possible to try to close it, however, if after manipulation, the hand is not well perfused, it is necessary to prepare for surgery to restore circulation immediately.
Nerve
Phải đánh giá cảm giác, vận động của mỗi thần kinh riêng lẻ trước và sau nắn: thần kinh quay ít khi tổn thương; thần kinh trụ hay bị kẹt phía trước hay dãn khi di lệch vẹo ngoài; thần kinh giữa có thể tổn thương khi trật khớp hay khi kéo nắn khớp khuỷu làm kẹt trong khớp.
SOME COMMON Clinical Tests
Back dislocation
clinical
Painful swelling in the elbow area after injury, marks of ax stroke behind the elbow, spring marks, jammed elbow joints, not pronation, arm axis does not cross the elbow when viewed from the side, changes in the vertices of Nélaton's triangle.
The treatments
- - Sealed:
- Many techniques for posterior dislocation of the elbow, the goal is to shift the elbow process anteriorly.
- Pharvin places the patient on his stomach and then applies manipulator traction. After a few minutes of pulling, the tip of the elbow slides into the fossa.
- Meyn and Quigley also placed the patient in a prone position with the arm on the table as counterweight, causing the forearm to swing rather than the entire arm.
- Kocher's new elbow dislocation technique is the smoothest and most correct elbow dislocation mechanism:
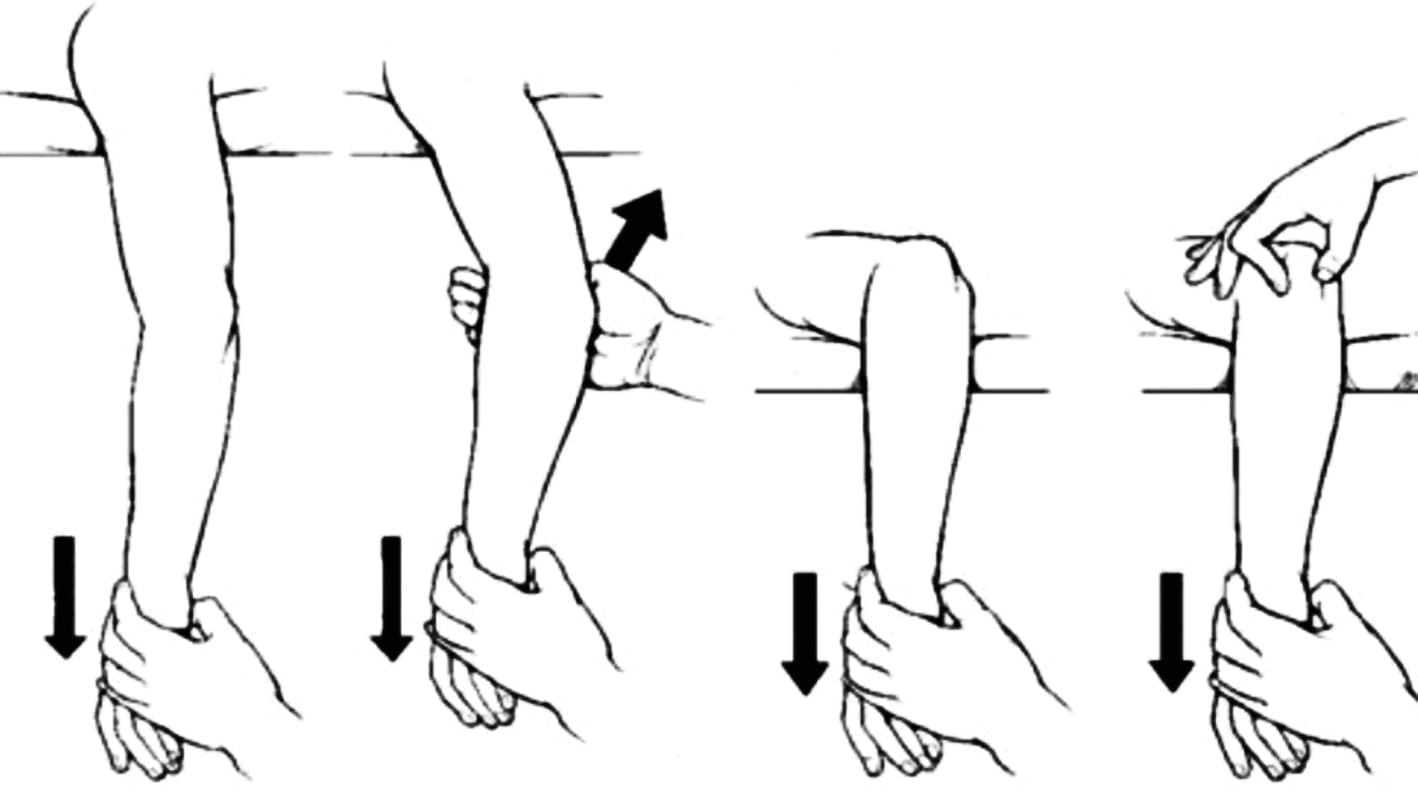
Pharvin Meyn and Quigley
Figure 10.2. Pharvin and Meyn and Quigley Elbow Technique [1]

Figure 10.3. Kocher's lateral dislocation technique [2]
- Post-manipulation check post-manipulation stability, usually apply a posterior brace with the elbow flexed at 90°. Most postmandibular stabilizers allow gentle active movement exercises in both flexion and pronation of the forearm after the first week.
- Open manipulation: rarely need to open the acute elbow dislocation, usually open when the dislocated elbow cannot be manipulated due to soft tissue jamming and locking the joint, sometimes the upper pulley can jam the joint.
Anterior dislocation of the elbow
clinical
- The arm appears to be short, with the forearm turned upside down
- The lower end of the humerus is prominent behind the elbow
- The biceps tendon stretches the skin in front of the elbow like a "tent stretcher"
- This form is often accompanied by an elbow fracture.
Treatment
- Temporarily brace the elbow to motionless in arm brace:
- Kéo nhẹ nhàng cẳng tay để giảm co cơ rồi đẩy đầu xa xương cánh tay ra trước, gấp khuỷu lại để bất động tạm ở tư thế < 90°.
- If there is a fracture of the elbow, it must incorporate stable bones.
Dislocated elbow to the side
- A ulnar elbow dislocation is usually a subdislocation rather than complete.
- Joint space wide, relative arm and forearm length normal.
- Manifest by bidirectionally pulling the forearm and distal to the forearm in a slight extension of the elbow, and then pressing the medial or lateral to a posterior dislocation.
SYMPTOMS
- Ligament calcifications
- Osteoarthritis
- Nerve - blood vessel compression
- Syndrome cavity compression
- Recurrent dislocation
- Stiffness
- Loose joints are seen after elbow surgery.
SLEEP SHOCKING
ANATOMY
Joints
- Shoulder joint (caps of arms – pan shoulder blade) is a fully movable joint. The socket is much smaller than the head (# 0.54 socket/cap) arm
- Above the socket there is an arc with the crow, the upper limit of the shoulder joint and the medial of the crest
- The alveolar cartilage deepens the socket.
Joint cover
- Starting from the parietal cartilage to the anatomical neckline of the humerus. Capsular ligament is a thickened component of the joint capsule, including: superior - anterior, medial - anterior, inferior - anterior, inferior - posterior ligaments.
- In addition, there is the crow-brachial ligament.
Neighboring ingredients
- Spindle: muscle above the spine, under the spine, small round, below the shoulder
- The biceps tendon passes between the biceps groove and attaches to the superior border of the socket
- The triceps tendon attaches to the tubercle below the socket
- Bundle of blood vessels, axillary nerve: goes under the cranium into the axillary socket, depending on the crow - arm muscle, just anterior - below the shoulder joint. The musculoskeletal nerve: penetrates the brachiocephalic muscle to enter the anterior brachial region 2 - 3 cm from the crow's apex.
INJURY MECHANISM
- According to Rockwood, there are two mechanisms that cause shoulder injuries:
- Direct: force applied proximal to humerus (very little)
- Indirect: still the most common.
- The combined impact force: form - extension - rotation outside the shoulder joint will lead to anterior dislocation of the shoulder.
CLASSIFICATION OF ANterior dislocation of the shoulder
According to Rockwood classification as follows:
- According to the degree of stability: misaligned and semi-disordered
- By progression: congenital, acute, chronic - trapped, recurrent
- According to the force of impact: trauma, natural, non-traumatic
- According to the patient's contribution: voluntarily, not voluntarily
- In the direction of dislocation: under the crow, in the crow, below the clavicle, below the shoulder.
DAMAGE Around the KITCH
Injury to the tip of the humerus
In 1940, Hill-Sach fully described: when the head of the humerus is displaced anteriorly in external rotation: the lateral part of the socket will be compressed and subside to become a "compression fracture", then the anterior margin of the socket like a sharp ridge to the cancellous bone at the back of the surgical neck and the top of the forearm.
Anterior capsule injury
- This lesion was fully described by Bankart (1939).
- Soft tissue injury is an anterior detachment of soft tissue structures from the socket due to displacement of the humeral head during dislocation.
Other Injury
- Injury to the rotator cuff can occur, or tear, stretch ligaments, joint capsule
- It is possible to break the great trochanter because when the arm tip is forward or downward, the counterbalance muscle group is still active to hold the great trochanter.
- Similarly, posterior dislocation can fracture the minor trochanter.
FREQUENCY
- This is the most common dislocation of the adult joints (accounting for 45%).
- Most are dislocated anteriorly, very rarely posteriorly.
DIAGNOSE
Medical history
- Mechanism of injury, arm posture, direction of force in the event of an accident
- The level of force determines the assessment of injury (De Palma's degrees I, II, III)
- Exploiting the patient's living and working habits.
clinical
- Clinical examination of anterior shoulder dislocation can be diagnosed: the patient is very painful, the arm cannot be let go, and must be supported or lifted with the other hand.
- Displacement below through, under the blow:
- Square shoulder sign, "axe-shy" loss of delta-thoracic groove. Empty joint.
- The “spring” sign (+). Arm slightly splayed, externally rotated.
- May damage nerves and blood vessels
Subaxillary dislocation: more damage to the capsular nerve vessels.
Additional Notes
- Tests to evaluate recurrence:
- Stress test, (Crank apprehension) postural fear of dislocation; Fulcrum test: dislocation first, permanent subluxation
- Feagin's, Sulcus's test – misses to the bottom. In a certain position.
- Concomitant injuries should be carefully evaluated:
- Nerve damage (especially the capsular, neuromuscular) by motor and sensory examination of the shoulder
- Vascular Injury: Need to evaluate for minor lesions or axillary artery occlusion
- Injury to the bone (greater anterior cruciate) and rotator cuff, anterior alveolar margin, joint entrapment.
X-ray
- Posture X-ray evaluation:
- Anterior - posterior X-ray: straight plane of shoulder joint
- True anteroposterior X-ray: clearly visible joint space.
(The center light head is facing out 45°, the film behind the shoulder is perpendicular to the head).
Axillary slant plane: survey the direction of dislocation, alveolar socket: the patient is axillary, radiating into the axillary cavity, head and shoulder film or curvilinear film focuses on the sacroiliac process.
The inclined plane shows the direction of dislocation and the alveolar margin, the socket neck: the patient stands, leaning against the wall, close to the film. Posterior X-ray, parallel to the shoulder blade from head to front, focusing on the top of the arm).
- Radiography of the rotator cuff in maximal assessment of Hill-Sachs lesions. (Arms rotate inward, close to body).
Lamp head tilted 15° outward; Arm swing in hand to behind. Lamp head straight (Hermodson pose) from the front.
In addition, there are many other positions to survey all shoulder injuries.
MRI and CT-scan
In addition to bone lesions, CT-scan and MRI also help to examine the rotator cuff, the parietal cartilage.
TREATMENT
No surgery
- Most acute traumatic dislocations can be treated conservatively with manipulation and immobilization.
- There are many different methods of straightening and are recorded very early (several thousand years BC, on Papyrus). For example: Hippocrates, Galen, Kocher, Milch – Lacey, Stimpson, etc.
- Regardless of the method, the dislocation must also be based on the mechanism of injury and the direction of dislocation. The patient's position, the force exerted by the manipulator, the counterweight of the assistant, the form of manipulation will depend on the above factors. The immobilization of the shoulder joint is short or long (2-4 weeks) depending on the injury of the shoulder dislocation. Rehabilitation The shoulder joint is crucial to avoiding recurrent dislocation of the shoulder.
Anterior shoulder dislocation
Hippocratic method
Bệnh nhân nằm ngửa trên sàn nhà hoặc giường thấp. Người nắn dùng hai tay kéo cẳng tay bệnh nhân theo trục cánh tay trong tư thế dang. Lực kéo liên tục tăng dẫn, đồng thời dùng gót chân đặt vào hõm nách bệnh nhân làm điểm tựa lòng bàn chân ôm lồng ngực bệnh nhân. Sau một lúc kéo để chỏm xương cánh tay xuống gần bờ ổ chảo, cho khép cánh tay bệnh nhân vào, đồng thời dùng gót đưa chỏm vào ổ chảo, khi khớp vào, sẽ nghe tiếng “cụp” (vì chỏm phải trượt qua bờ ổ chảo) và bệnh nhân cảm thấy dễ chịu, nếu bệnh nhân tỉnh, không gây tê ở khớp. Kiểm tra lại không còn thấy dấu hiệu trật khớp.
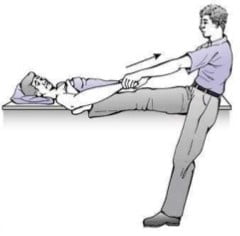
Figure 10.4. Hip dislocation according to Hippoccrate [3]
Kocher's method
Patient position: sitting, elbow flexed. Consists of four steps:
- Step l: repeatedly pull the arm in a slightly outstretched position (spring jam position)
- Step 2: Rotate the outer arm gently until 80°, still pulling continuously
- Step 3: Keeping the arm in an external rotation position, bring the elbow forward near the midline of the body, still pulling continuously
- Step 4: Rotate in the arm so that the hand rests on the other shoulder. The patient feels that the joint has been straightened, feels comfortable, no pain, no spring symptoms. Check the shoulder joint for easy dislocation.
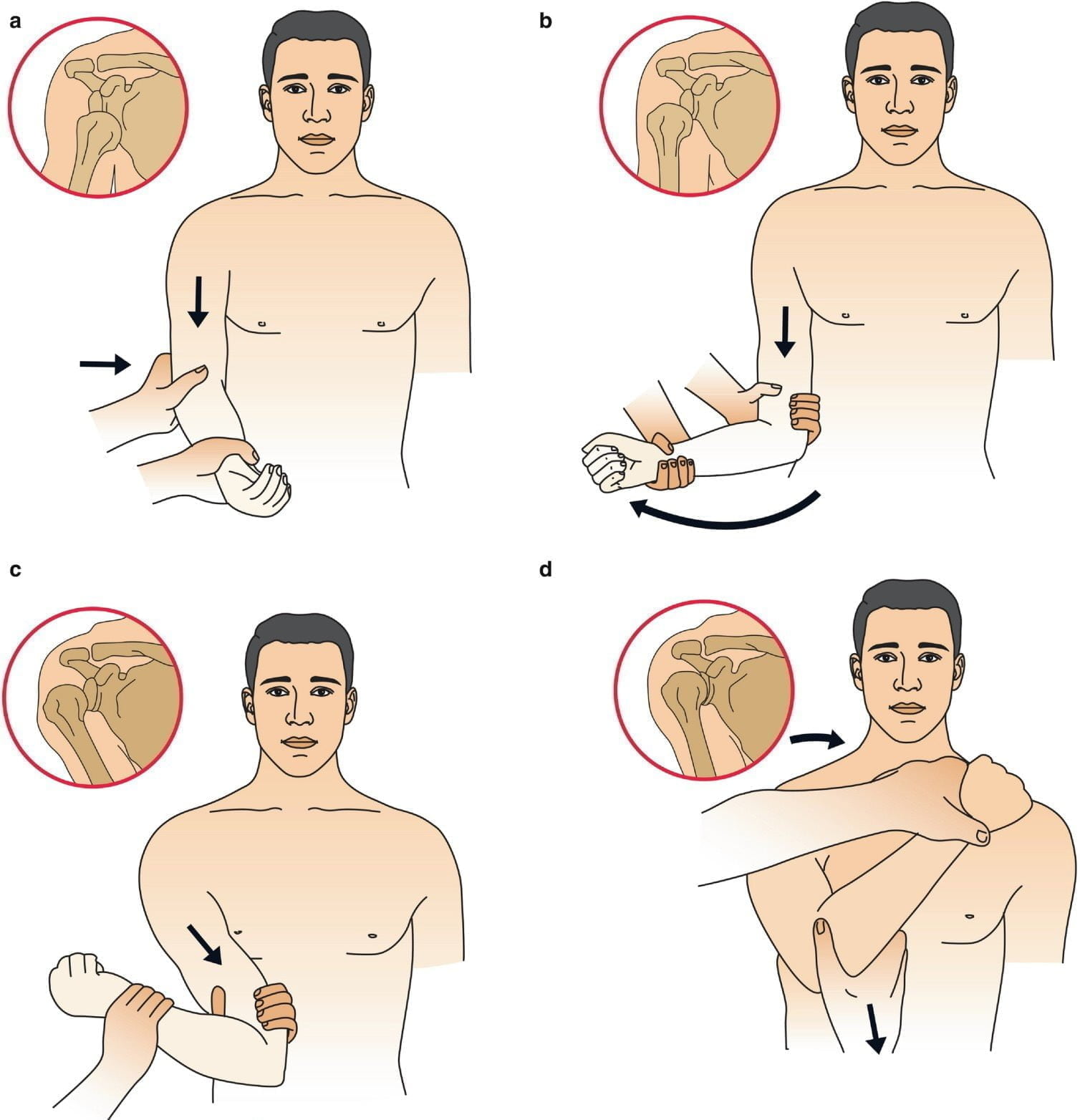
Figure 10.5. Shoulder dislocation according to Kocher [4]
Surgery
- Point:
- When there is a situation where the joint cannot be closed
- Or recurrent dislocation of the shoulder.
- When opening, it is necessary to restore the muscles under the shoulder, under the spine, and in the joint capsule.
- Surgical treatment of recurrent dislocation of the shoulder is based on reconstruction of damaged anatomical structures.
- Methods may include:
- Bankart surgery: restoration of the anterior capsule and the anterior margin cartilage
- Jobe surgery: repair of the capsule – with cut and suture of the capsule according to the letter T
- Du Toit surgery sews two layers of joint capsule with special needles
- Putti-Platt surgery: reconstruction of the subscapular muscle or repositioning of the subscapular semi-tendon
- Magnuson-Stack surgery: transferring the attachment of the tendons under the shoulder simply
- Eden-Hybbinette surgery: wedge the bone to the anterior margin of the hollow socket with the tibia, iliac crest
- Connolly surgery: transferring the attachment site of the subspinous tendon to the defect of the superior humerus or defect due to Hill-Sach's lesion
- Trillat surgery (Coracoid transfer): moving the crow's process downward and outward to fill in the anterior margin of the defective socket.
In addition, there are many other surgeries: Bristow - Helfet, Latarjet, Nicola, Gallie, Saha, Boytcher, ... Bristow - Latarjet surgery is the simplest of all.
SYMPTOMS
Complications of shoulder dislocation
- Nerve damage:
- Level of injury: three groups
- Neurogenic edema (neuropraxia): fully reversible in 1-2 months
- Axonotmesis: the axonal sheath should heal itself by 1 mm/day
- Neurotmesis: Needs to be cut and sutured to restore nerve.
- There are many records of the extent and frequency of nerve damage.
- The plexus can be completely paralyzed, but the most common frequency is the axillary cord, followed by the external dermal muscle cord.
- Level of injury: three groups
- Vascular injury: there are many degrees: small branch rupture, thromboembolism, endothelium injury or rupture.
Complications right after pressing
- Posterior lateral lesion of the bony crest (Hill-Sach's lesion)
- In addition, soft tissues can be inserted into the articular surface such as the biceps tendon, the detachment of the great trochanter, the subscapular muscle, the marginal cartilage, and the capsule.
Complications after treatment
Dislocation occurs if immobilization is not correct and physical therapy is lacking to restore shoulder function. Reversible dislocation is possible despite proper immobilization due to the extent of the damage to the crest and capsule, the brachial head, and the alveolus.
Other Complications
Inflammation around the shoulder, osteoarthritis, periarticular calcification, stiffness, shoulder-hand syndrome.
GRAPHIC DISCLAIMER
OUTLINE
- Hip dislocation is uncommon, accounting for less than 5% of total dislocations. The male:female ratio is 5:1.
- The hip joint is stable, anterior and posterior have pelvic columns located around the hollow, these columns are very strong, so the force of injury must be strong.
- When the head is dislocated, it breaks the posterior border above the joint cavity, causing damage to the sciatic nerve, dislocating anteriorly and also injuring the obturator femoral nerve.
- Hay kèm thương tổn gối cùng bên nhất là bị vỡ xương bánh chè, rách dây chằng gối.
- Or have late sequelae:
- Necrosis of the femoral head circuitless
- Arthritis groin after injury
- Need to straighten as soon as possible. Any late hour will add more sequelae than that hour.
CLASSIFY
General classification: according to Stewart there are two ways of classifying:
In the wrong way
- Rear dislocation: very common, up to 4/5 total dislocations include:
- Backward, upward: the most common type
- Backward, downward: sitting style
- Displaced first: rarely seen
- Front out, up: mu style
- Overturned front, down: seal type.
- Central dislocation: acetabulum ruptured, the crest sunk deep into the hollow bottom. Cause: due to a car accident, the car stopped suddenly, the knee hit the wall of the car, the head hit the acetabulum and broke the acetabulum.
According to the weight
- Grade 1: Simple dislocation, acetabulum intact.
- Grade 2: The socket is chipped or broken, the small curtain is still stable.
- Grade 3: The acetabulum is broken into large pieces, easy to insert, the joint is not stable, and it is easy to bounce back.
- Grade 4: Dislocation with broken crown or femoral neck fracture.
GENERAL CLINICAL SIGNS
Dislocated joints always show signs of elastic resistance (spring marks). Generally speaking:
- Posterior dislocation: thigh closed
- Anterior dislocation: thigh shape
- Upward dislocation: thigh slightly flexed
- Displacement downwards: thighs are flexed much.
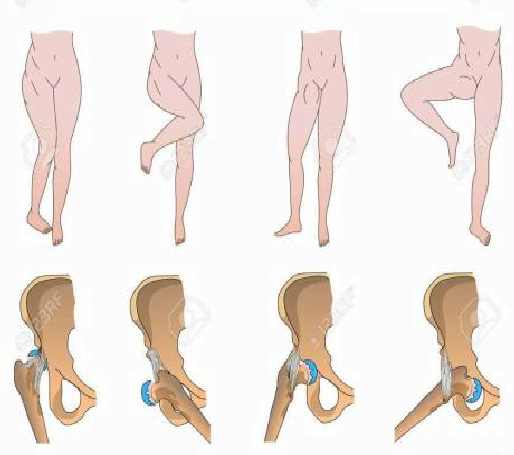
Figure 10.6. Clinical forms of hip dislocation [5]
Thus, for example, in the posterior-upward dislocation, the very common pelvic type, we see the thighs closed, the knees slightly flexed. Pubic dislocation: flexed thighs, flexed hips, etc. if accompanied by broken neck, broken femur body clinical symptoms will not be obvious.
Dấu hiệu liệt thần kinh:
- Great sciatic nerve palsy: numbness in the soles of the feet
- Fetal nerve palsy: numbness of the anterior medial side of the thigh.
When suffering multiple injuries, a lot of shock must take care of general resuscitation, it is cold to cover with a blanket, so it is easy to miss the injury. But if you leave it too late, the end will be very bad. In general, with multiple trauma, when taking cranial and abdominal scans, additional imaging should be required:
- Bilateral hip joint
- Lumbar thoracic spine.
KITCHEN DISCLAIMER
General principles
- The more severe the injury, the worse the outcome
- Need to straighten before 12 o'clock, whether closed or surgical
- Only squeeze 1-2 times only. Insensitive, soft and gentle. Rough manipulation damages the cartilage of the head, causing a fracture of the femoral neck.
- If it is not achieved, it will be operated on.
Steps to take
- Preoperative CT scan clearly shows bone damage, but it should be straightened first, not waiting for CT results to waste valuable time.
- Anesthesia should be given, even for muscle relaxation (needs anesthesiologist) for muscle softening. It's fine in the operating room.
- After straightening, re-examine the sciatic nerve, sometimes the nerve is paralyzed when straightening.
- Take a check after straightening, need to see if the tip is right in the joint cavity, the line is bright
Is the edge of the crown even? Only slightly eccentric, with a slightly wide light slit, one immediately thinks of a small piece of cartilage, a torn piece at the edge of the acetabulum stuck into the joint slot.
In doubt, a CT scan should be performed after manipulation. If there is a piece stuck in the joint space, it should be surgically removed. For small pieces, it can be delayed without immediate emergency surgery.
Method of straightening
- Sealed:
- Backward: conforming to Allis, Bigelow
- Flip out first:
-
- Pub type: straight pull
- Clamping type: Pull – Gradual Fold – Rotate – Pull thigh from inside to outside Allis
-
- The Allis maneuver (posterior hip dislocation) (Figure 10.7) is most commonly used: the patient is supine, under general anesthesia, and the two iliac spines are fixed to the bed with a belt or by a person holding them down. Bend the knee 90°, thread the #8 cloth belt under the patient's hip and drape it around the physician's neck. Bend the doctor's knee under the patient's knee as a lever support, gently press the patient's ankle down, the doctor slowly pulls the thigh straight up to the sky, sometimes adding a slight rotation.
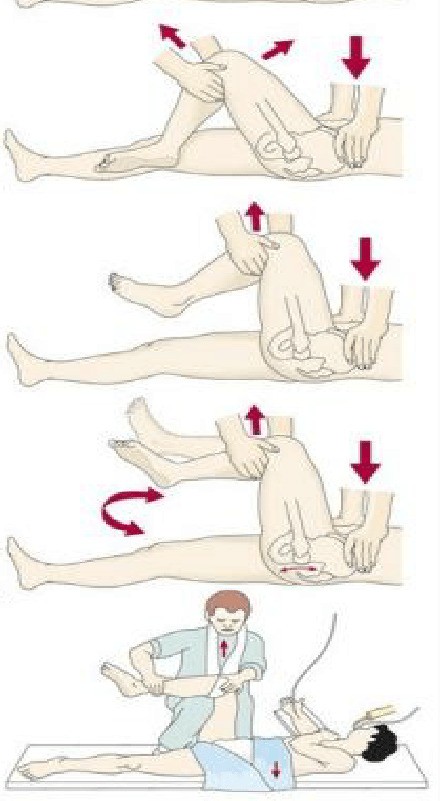
Figure 10.7. Allis-based hip dislocation [6]
-
- Don't let your back be scared caseation the tip, usually avoid it for 2-3 months, sometimes see the necrotic tip in 6 months, avoid much pressure and hope to regenerate the tip.
- Bundle of dough do sợ hoại tử chỏm, sợ trật lại. Một số bó bột 4 – 8 tuần.
- Pull continuously to support the pressure on the crown. Pierced light weightlifting 2 - 6 weeks.
- Scaling:
- When surgery is required, incisions can be made in front and behind. The anterior entrance is more likely to have a pulseless peak.
- It is usually better to operate on the back. Kocher Langenbeck incision.
Complications and Prognosis
Sunshine hour
Need emergency care early every hour. More than 24 hours late, the results are bad because the circulation is often damaged.
- Over 262 follow-up cases showed:
- Premature treatment before 12 hours, avascular necrosis 17.6%
- Late healing after 12 hours, with avascular necrosis 56.9%
- Hougard said:
- Preset 6 hours, avascular necrosis 4%
- After 6 hours, avascular necrosis 58%
- Comparison of non-surgical and surgical manipulation shows:
- Sealed without surgery, had avascular necrosis 15.5%
- Healed by surgery, got avascular necrosis 40%
Do not give it early because the tip is "sick"
Sooner or later, however, little difference is seen. Brav with 523 cases:
- Given 12 weeks before, had avascular necrosis 25.7%
- Give the spleen after 12 weeks, have avascular necrosis 26.6% When you feel pain when walking, do not give the spleen.

