DEFINE
Sprain (English is ) spain) is a folk word (accepted by the Vietnamese medical profession as a scientific term) for the major (usually closed) injuries of the ligaments that hold the joint firmly. Usually accompanied by joint capsule damage in general. Sometimes damage to the muscles that hold the joint steady can also be seen. The sprain is completely unrelated to the tendon injury alone.
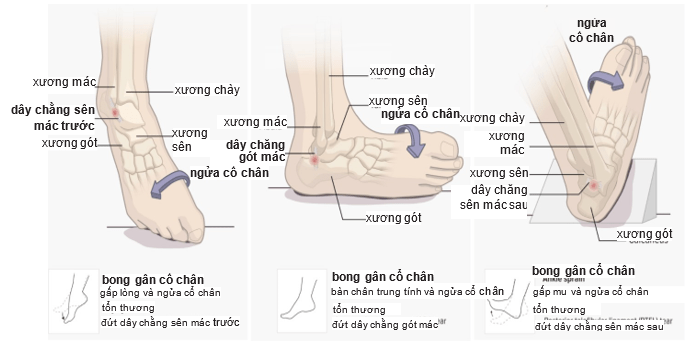
Figure 9.1. Sprains of the peroneal and calcaneal ligaments [1]
MECHANISM
It is usually an indirect injury in the direction of twisting or flexing, causing the contralateral joint space to widen and the ligaments to be overstretched and injured. Sometimes the mechanism is complex including twisting and folding. Severed ligaments are not classified as sprains.
Anatomy – Pathophysiology of the Microscopic Pathology of the String
After a ligament injury, we see a three-stage process (according to Oakes):
- The acute inflammatory phase, lasting about 72 hours, is seen with rupture of blood vessels and infiltration of blood into cells.
- The recovery phase, which takes place between 72 hours and 4-6 weeks, has collagen accumulation at the sprain area.
- The period of rebuilding of ligaments and other tissues, which occurs from 4-6 weeks after injury to 3-6 months [even up to 12-16 months, (according to Sisk)] is the period of collagen reorganization. and muscle.
Acute inflammatory phase
Manifested mainly by the rupture of small blood vessels, red blood cells escape from the blood vessels and formation of fibrin clots in the sprained area. Within 36 hours, polymorphonuclear monocytes and macrophages were mobilized to the injured area. Mast cells and other cells release histamine serotonin and prostaglandins, which, in turn, cause maintenance and extravasation of blood leakage. The capsule responds with aseptic capsulitis following trauma, as described above.
Recovery phase
Manifested by hemolytic inflammation. Macrophages destroy dead cells, red blood cells, and blood clots. Simultaneously, vascular buds appear, from which new microvasculature and fibroblast transport occur. Collagen fibers are formed (Wolf's law progression is the same as that of ) bone healing fracture) gradually enlarges (increase in diameter) and gradually increases even the minimum tensile strength and also after that time the collagen fibers can withstand the tension without breaking again. At this stage, collagen fibers have not developed in accordance with the direction of tension.
Regeneration phase of ligaments and other tissues
The process of growing collagen fibers continues to slowly take up to 12-18 months to complete. At this time, the new collagen fibers grow in the direction of the stretch. Directed collagen growth depends on the above-mentioned proper treatment. If treated incorrectly, collagen fibers will grow messy, not oriented, causing sticky scars. Recent studies have shown that careful, guided, and controlled exercise, as well as minimal mechanical (stretching) activity of the ligaments at the right time, will stimulate
Improves the synthesis and regeneration of collagen fibers as well as enhances the tensile strength of ligaments.
STATISTIC FIXING FACTORS AND MOBILE FIXING FACTORS
From the classical point of view, it seems that only ligaments are responsible for holding joints.
According to today's knowledge, there are two types of factors that hold the joint:
Static stabilizers
Includes classic ligaments. Today, capsular ligaments are also added and are called capsular ligaments.
Dynamic stabilizers
Includes the tendons and muscles that surround the joints.
All of these elements work synergistically to stabilize the joint, and there are often many elements that work together to keep the joint stable. For example, in the past, the classical notion that there was only cruciate ligament The anterior is responsible for preventing the tibial plateau from moving forward. Today, knowledge shows that many factors are involved in this task, including:
- Ligament front cross
- Anterior medial capsular ligament bundle
- Pelvic – tibial strip
- Biceps muscle
- Back horn of meniscus.
Since then, the concept of ligament damage has also changed from the previous rudimentary concept. If it is a third degree sprain, it is rarely just a single ligament injury. Because if you want to completely break a certain ligament, excessive movement of the joint is enough to damage other elements adjacent to that ligament to varying degrees. Therefore, it is necessary to fully diagnose all lesions to recover well.
Other strengthening factors may be used to increase the effectiveness of certain ligament injuries. For example, for anterior cruciate ligament rupture, in addition to the rehabilitation treatment of that ligament, one can also strengthen the biceps muscle and the iliotibial band (also a muscle) to increase efficiency. treatment results.
CLASSIFY
Major ligament and capsule injuries are divided into three grades:
- Grade 1: Sprain: Lesions that tear only a minimal number of fibers of the ligament, so it is sometimes considered that the ligament is only stretched. The anatomical damage was considered insignificant.
- Second degree sprain: There is a tear in more fibers of the ligament, so it is sometimes considered a ligament tear.
- 3rd degree sprain: A completely ruptured ligament loses its continuity and causes joint dislocation. There may be a purely ligamentous rupture (often accompanied by a tear of the adjacent capsule) or may dislodge a piece of bone in the upper or lower end of the ligament attachment. The most severe degree of 3rd degree sprain will lead to dislocation. It is damage of many ligaments and extensive damage in one joint.
For grade 1 and 2 sprains, the ligaments are still continuous and have not caused joint dislocation.
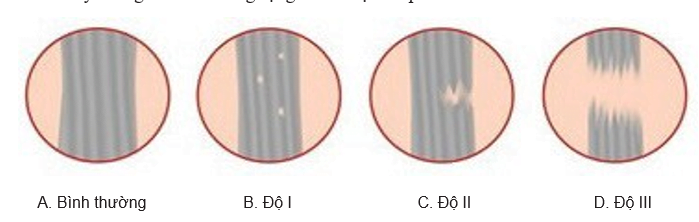
Figure 9.2. Sprain grades [2]
CONSISTENT DISTANCES
The most common disorder is posttraumatic aseptic bursitis, a reactive inflammatory type of synovial bursitis. Post-traumatic bursitis accompanied by joint effusion, manifests in two forms:
Serous effusion
Joint socket water is lemon yellow, clear. Joint fluid has a low albumin content (3-1%), consisting mainly of transudates. Microscopic examination of the smear showed a few white blood cells.
Hemorrhagic synovial joints
If the sprain is accompanied by a broken blood vessel. Blood water mixed with serum. If there is a lot of bleeding, a joint puncture shows only complete blood. Only a few hours later, there will be inflammation, bleeding, or inflammation that recovers with all the signs of natural pain, swelling, redness, and heat in the joints. Due to pain, the joint contracts in response to the pain-resistant deformed position. If not properly treated in a grade 2 or 3 sprain, post-traumatic bursitis will become chronic and persist for a long time. Although a ligament is a soft structure, it must be very strong and of the right length to limit unnecessary or harmful joint movements. Ligaments that are torn (grade 2) or completely broken (grade 3) need to be restored to both their original length (no longer) and strength, to withstand tension. If the above-mentioned recovery requirements are not met, the joint movement will warp, causing pain, and prolonging bursitis. It is chronic aseptic bursitis, joints will have reduced function, can not function normally because of pain and very difficult to treat.
DIAGNOSE
Diagnosis is based on:
- Ask medical history
- Clinical signs
- Sometimes there are pictures X-ray, but X-rays are not always helpful in diagnosing a sprain.
Medical history
Often the typical mechanism of injury is torsion or angulation, or both.
- Sharp pain "like an electric shock" when injured
- Numbness (no pain) for a few hours
- The pain returns more and more, even though the joint has been motionless. Hearing a "crack" sound when an accident is a complete rupture of the ligament.
Clinical signs
Localized edema, edema if present early is severe sprain. Occasionally accompanied by bruising due to localized hematoma where the ligament is injured, if present, the diagnosis is easy. Sometimes it's just a general joint effusion.
- Pain: natural pain of the nature described above. Discomfort when pressing on the damaged ligament or pain along the entire ligament or just sharp pain when pressing where the ligament attaches to the bone. Pain increases when we open the joint on the side of the injured ligament.
- Movement of the joint space more than the healthy side will be obvious if it is a 2nd degree sprain, especially a 3rd degree sprain. For example, a ruptured case lateral ligament pestle (inside) knee joint If we do a shin movement (dissecting the internal joint space), we see a larger variation than the healthy side.
- The clinical signs of traumatic bursitis are quite obvious
- Swollen joints
- The joint capsule feels thicker than usual, filled with fluid, lost the hollows around the joint, painful, and slightly hot
- Aspiration will determine the type of effusion.
X-ray
Not every sprain has a typical X-ray appearance. X-rays are diagnostic only in the following sprains:
- Injury to ligaments at the site of bone attachment: X-ray shows a conventional fracture.
- Grade 3 sprain: must be taken in the forced open joint position (dynamic X-ray). Anesthetize the joint to relieve pain, put it in the open position of the joint on the side where the ligament is broken when taking X-rays. Take the opposite side of the joint in the same way as mentioned above. The extent to which the joint gap is wider than the healthy side will allow the degree of joint dislocation to be determined.
Magnetic Resonance (MRI)
Identify the specific injury to the capsular ligament. The diagnosis must clearly define:
- Is there a sprain of which ligament (or of which ligament)
- Degree of sprain
- Accompanying injuries (fracture, overflowing joints, ...) then the right treatment can be determined.
TREATMENT
Treatment has two purposes:
- Treatment of acute inflammation after trauma
- Repairs and regenerates injured ligaments (and muscles). Thus, for grade 1 sprains, only acute inflammation after the injury is enough, because the anatomical damage to the ligament is considered insignificant. Conversely, for a grade 2 or 3 sprain, both requirements must be fulfilled. If treatment to restore and regenerate the ligaments is not good, the bursitis will become chronic and permanent.
Treatment of acute bursitis
- The goal is to limit bleeding to a minimum, thereby limiting the formation of edema due to extravasation of blood and reducing pain. Detail:
- Things to do:
- + Let the sprained limb lie still
- + Apply ice (if not available, apply cold water) every 20-30 minutes, for 4 hours immediately after the injury
- + Continuous compression for at least 48 hours
- + Elevate the injured limb to stimulate favorable venous circulation and rapidly drain the hematoma.
- + Use anti-inflammatory drugs such as drugs that block prostaglandin secretion (such as Indomethacin, ibuprofen, ...) immediately after the injury or within 24 hours at the latest to limit the formation of edema
The above measures, especially applying ice, will relieve pain quickly.
- Things to avoid not to do:
- + Do not apply hot (any way), at least within the first 42-78 hours after the injury. Since heat also eases pain, many people make the mistake of making it. Heat will dilate blood vessels and also increase blood outflow and increase edema
- + Do not let the patient drink alcohol, which is also a vasodilator
- + Do not inject anesthetics, steroids, hyaluronidase or a mixture of such substances into the sprain area because the above drugs, especially steroids, can slow collagen recovery (according to Oakes' research). If done poorly, it can easily cause infection
- + Do not massage or exercise the sprained area in the acute inflammatory phase. Doing so only causes further damage, further bleeding and edema.
Treatment and rehabilitation of ligaments
The best way to restore torn or ruptured ligaments is to bring the ruptures together to restore their original length and to immobilize protection as long as the ligament is not fully healed. Thus, for a grade 2 sprain, simply immobilize protection for enough time (4-6 weeks). For grade 3 sprains, it is best to have early surgery to suture the ligaments and be immobilized for enough time. Early mobilization is only allowed (after 2-4 weeks after surgery) if it is guided and controlled by a qualified and experienced physical technician, with minimal and cautious movements. If you can do that, the regeneration of the ligament is better.