Table of contents [hide]
BREAKING FLEXIBLE NECKLACE
Outline
Fracture of femoral neck (femoral head fractures) is one of the cases fracture lower extremities whose fracture line is midway between the crest and the trochanter. Common in the elderly, even a minor injury (such as a fall on the buttocks). Very rare in young people and children. Prognosis of bone healing quite complicated by prosthetic joints and resorption. Often life-threatening by complications such as pneumonia, urinary tract infections, heart failure, sores from lying down for a long time.
Recall important anatomical elements
The weak point lies between two skeletal systems: the base fan system and the pointed arc system.
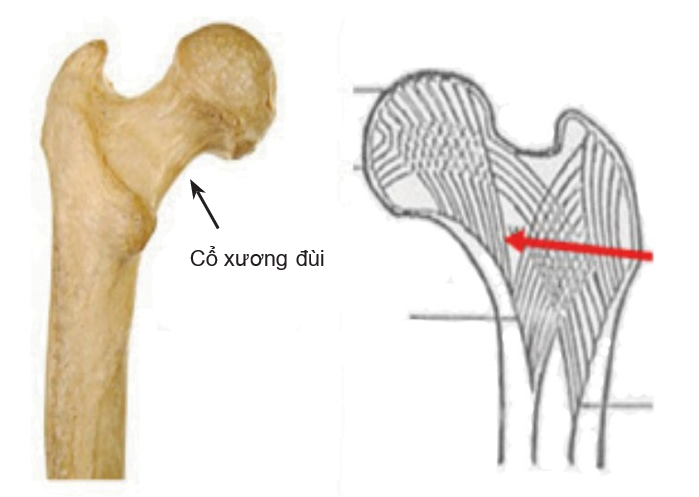
Figure 6.1. Weakness at the junction between two skeletal systems [1]
- About X-ray
Sealed neck arc: is a continuous arc connecting the femoral neck margin and the superior obturator ridge.

Figure 6.2. Sealed Neck [2]
- Neck angle: is the angle formed by the axis of the femoral neck and of the femoral body.
Normally the angle is about 130o.
- About the capillary feeding circulation
Upper group: is formed from 3-4 small branches branching from the internal circumflex artery, connecting with the external capsular branches, obturator branches, the branches follow the joint capsule to nourish the upper space of the cap.
Inferior-medial group: separated from the internal circumflex artery feeding the inferior 1/4 of the cap.
Round ligament artery: separates from the obturator artery, has a very small role to nourish only part of the crest.
Classify
According to Garden: based on existing relationships of longitudinal bone fibers. If the correlation is maintained, then the displacement is less important and the cap nutrition is good thanks to the intact joint capsule. The prognosis will be good.
- Team: Fracture a bone shell.
- Level II: Whole bone fracture, no displacement.
- Grade III: The whole wall of the bone is broken, partially displaced, and the two fracture faces are still pressed against each other.
- Grade IV: Completely displaced fracture, the head of the bone is free in the acetabulum. Ratio caseation high crest.
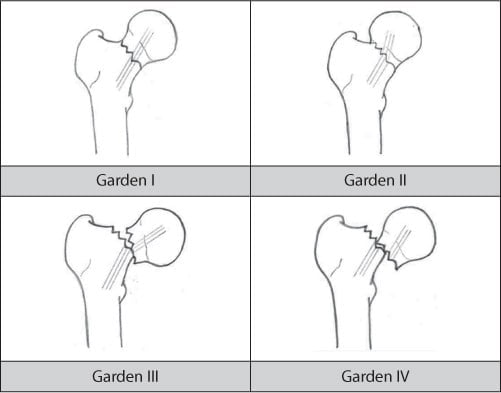
Figure 6.3. Garden Classification [3]
According to Pauwels:
Team: The broken line is made with the horizontal line at an angle equal to 30o, easy bone healing.
Level II: This angle is equivalent to 30 - 50o, the prognosis of bone healing is difficult.
Grade III: This angle is equivalent to > 50o, the risk of apical necrosis is high.
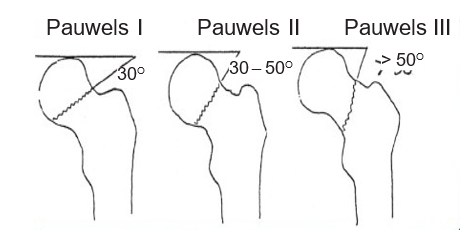
Figure 6.4. Pauwels grading [4]
Clinical symptoms
Depending on the type of fracture (annular or closed fracture), the clinical symptoms are different.
Leg fractures are officially closed fractures: common, the fractures are separated by muscle contraction. The lower fracture is in adduction and external rotation.
Location:
- Subcapsular fracture: This type of fracture is complicated to treat because only the crest is small. The crest is poorly nourished, only the round ligament artery remains, so bone healing is difficult, easy to lead to prosthetic joints or capsular resorption.
- Transcervical fracture: prognosis is better than the above type because there is still a part of bone attached to the head, better nutrition.
- Fracture direction: usually from bottom to top from inside to outside
- Displacement: non-interlocking fractures
- The distal segment is displaced upward by the gluteal muscle, the two bones are angled, at an angle downward and posteriorly.
clinical
- Pain: pain is most severe when trying to move the groin
- Complete loss of function: unable to lift leg off the bed plane
- Deformity: short broken leg, closed thigh, turned out foot

Figure 6.5. Common deformed posture (source: Author)
- Feel the large trochanter being pulled upwards
- There is a change in the line of Nélaton Roser, normally the anterior iliac spine is on the great trochanter, and the humerus is in the same line. At fracture of the great trochanteric trochanter, it is pulled upward, above the junction of the anterior superior iliac spine and the dorsal dorsum.
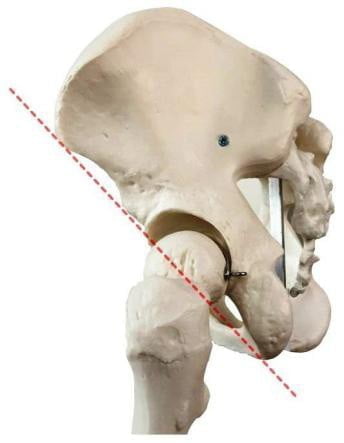
Figure 6.6. Nelaton Roser Road [5]
- There may be an effusion knee joint broken side.
X-ray: need to straighten and tilt the hip on the broken side.
Legitimate neck fractures form: Less common than closed fractures because the two segments are interlaced.
Clinical: After the fall, the mass of the trochanter fell to the ground, the bone was broken and the neck brace was made. The clinical symptoms are often unclear, the loss of function is not complete, the patient can lift the heel from the bed and in some cases still stand up, then the fracture may separate to become an adnexal fracture.
X-ray: subcapsular or transcervical fractures are almost transverse. Two interlocking fractures widen the neck angle
Progression and complications: with good treatment, systemic complications can be avoided, bones heal after 3-4 months, no sequelae. If the treatment is not good, it will leave many complications
- Early complications: trauma shock (rarely)
- Combined injury: acetabular injury or femoral shaft fracture
- Late complications.
Body
Ulcerative skin lesions, buttock ulcers, heel spurs
Cardiopulmonary damage: bronchitis, pneumonia, risk of heart failure Urinary complications: urinary tract infection
Thrombosis: phlebitis and pulmonary thrombosis.
In place
Deviation: in the closed hip position, the limb is shortened by 4-5 cm and can be compensated by scoliosis of the hips, spine, and high-soled sandals.
Bad luck: easy risk osteoarthritis especially hip joint, Spine. Prosthetic joints: due to treatment deficiencies such as motionless poor, early exercise.
The principles of treatment:
- Orthopedic method
Applied to braces fracture: these are the cases with good prognosis, the patient is not required to stay in bed. The patient can lift the heel and, if possible, walk. X-rays must be examined to monitor the fracture line. However, the risk of secondary displacement is so important that surgical intervention is required. Therefore, it is necessary to prevent secondary displacement.
Some surgeons treat it with bed rest and gentle leg movement.
Số khác lại khác thích cast chậu đùi để tập đi dần dần và giúp nhanh liền xương.
According to the classical treatment, people are treated with a Whitman cast, which is based on the breastbone close to the armpit down to the toes. When the powder is dry, let the patient practice standing, walking and leave the powder for about 3-4 months. However, because the powder is heavy, it is only applicable to healthy people.
Kéo liên tục: nếu không thể bó bột được, người ta xuyên đinh qua đầu dưới xương đùi và kéo liên tục trên khung Braun với háng dạng, bàn chân xoay trong. Tuy nhiên, do kéo bệnh nhân phải nằm lâu dễ có biến chứng toàn thân, do vậy ít áp dụng.
- Surgical method
- Indicated for all displacement fractures. These cases may heal spontaneously and progress to a loose prosthetic joint with a shortened limb and poor support on the limb. The goal of treatment is to avoid prolonged bed rest and thus either incorporate strong bones to allow for walking with crutches and progressive leg support on the broken side and exercise. Rehabilitation sớm, hoặc là phẫu thuật thay khớp háng để cho phép chống chân đi lại tức khắc.
- Bone fusion: first need to straighten on the orthopedic table with general anesthesia and X-ray examination.
- There are many surgical methods such as using nails, simple screws, DHS (Dynamique Hip Scew) compression screws, L splints, etc., after surgery, it is necessary to allow early exercise and gradually lean on the broken limb. Full leg rest when bone healing is evident on x-ray, usually 2 months after surgery. The surgical methods often depend on each school as well as the surgeon's habits.
- Hip replacement: total and partial.
- Prognosis
- Necrosis of the head can occur during the fusion time up to 2 years, especially in cases of fracture with displacement.
- Post-bone fusion prosthesis.
- Inflammation of the acetabulum due to prosthetic head, loose cement in the body of the prosthetic joint.
- Preventive
- Propaganda and education in the community about traffic and labor laws.
- Need to educate the community first aid Good localization of fracture cases to limit complications in fracture.
- For grassroots health facilities, it is necessary to diagnose early, treat properly and transfer to specialized medical care for early treatment to minimize complications due to femoral neck fracture.
- Educate patients on rehabilitation exercises after treatment.
BREAKING SHOCKET BACK
Outline
Fracture of the femoral shaft is limited from the inferior border of the great trochanter to the 5 cm superior border of the lateral condyle. The femur is a bone that has a unique resistance to injury due to its anatomical structure. It is due to the three physiological curvatures and the arrangement of the bearing zone. Because it is a large bone with many strong muscles attached to it, femur fractures are often caused by strong trauma, so they are easy to cause stunned which need emergency treatment is circulatory compensation and immobilization. Usually occurs in the working age 12 - 15% and today is encountered in many traffic accidents.
Fractures of the femur are classified according to the anatomy and location of the fracture line: upper 1/3, middle 1/3, and lower 1/3. For a fracture of the upper third close to the trochanter, it is difficult to distinguish a fracture of the trochanter. Pay attention to fracture of the lower third of the femur or intercondylar fracture, the treatment is quite complicated, complications of knee stiffness are likely to occur.
Anatomy physiology
Fracture at the top of the femur. The fracture site was in the area 5 cm below the baby's trochanter. This is a fracture site with many complex displacements due to strong pulling of muscle blocks in different directions at the top of the femur. The gluteal muscles are very strong attached to the great trochanter, and when contracted, the upper head is broken and rotated outward. The pelvic lumbosacral muscles attach to the trochanter, causing the upper head to bend forward. The result is a lot of cornering and displacement. The adductor and internal rectus muscles forcefully pull the lower segment inward and rotate it outward.
The 2/4 fracture in the middle of the femoral body has less complicated displacement compared to the upper fracture, the canal is narrow and cylindrical over a long segment, this property is more favorable for the application of intramedullary nailing than the upper part. apply other treatments.
Fracture at the lower end of the femoral body. The fracture line is usually horizontal or diagonal downward and forward. The upper fracture is susceptible to strong pulling and thrusting into the femoral extensor muscle mass, while the lower segment is pulled posteriorly by the twin muscle mass, thus easily causing damage to the posterior vascular-neural bundle.
clinical
Cause: usually due to strong direct trauma such as a traffic accident, or an indirect injury combined with folding and twisting. Common in adults and children 3 to 5 years old.
Fracture line: includes transverse fracture, diagonal fracture, torsion fracture, bilayer fracture, third fragment fracture or crumbling fracture.
Displacement: depending on the fracture location and has different displacement patterns. Common displacements are angular flexion, lateral deviation, short overlap, and lateral rotation of the distal fracture.
Clinical examination
The patient may have severe pain in the thigh area.
Complete loss of function, the patient is unable to lift the leg. It is important to think about possible shock for prevention and treatment.
On-site examination often reveals specific deformities: angular flexion, making the thigh look round by opening the angle inward, especially when breaking in the upper femur.
Big swollen thighs.
The limb is usually short compared to the healthy side.
The foot is externally rotated, the lateral margin of the foot is close to the patient's lying plane. For low fractures, because the distal fracture tip is pulled back, it is easy to insert into the vascular bundle, nerve, and popliteal socket, so it is necessary to clearly determine whether there is damage to blood vessels, nerves or not. Pay attention to flexion and extension of the foot or the loss of sensation in the soles of the feet and a small anterior ankle in case of compression of the sciatic nerve. In addition, it is necessary to carefully examine the hip and knee area to detect combined injuries such as acetabular rupture, hip dislocation, fracture cruciate ligament sau, vỡ xương bánh chè.
Need to carefully examine the feet to detect lesions caused by multiple injuries. Pay attention to the skull, spine, and intra-abdominal visceral rupture.
X-ray
Although an x-ray diagnosis is essential, a thorough clinical examination is necessary to avoid missing lesions. In some cases, hip dislocation or supraclavicular fracture associated with femoral shaft fractures were missed because of limited imaging of the fracture. Therefore, in order to have a good X-ray film, it is necessary to pay attention to:
- Capture two joints of the fracture head in at least two planes, straight and inclined.
- Bone scan of the healthy side for comparison if necessary (usually applied to children).
Symptoms
Shocked
Dizziness can be transient through pain relief by good temporary immobilization, this shock is usually due to pain. Shock may be caused by blood loss of the fracture, the thigh circumference should be measured to estimate, if the thigh circumference is too tight compared to the healthy side, it can be more than 500 mL in a 50 kg person.
Loss of pulse in the hamstring and ankle
- The cause of femoral artery rupture or compression of the most distal fracture is fracture of the femoral head and supracondylar fracture. Or it may be because blood from the fracture spills into the popliteal artery. Symptoms may present with pain in the lower legs, numbness in the extremities, cold feet, and very tight hamstrings.
- When a popliteal compression or rupture is diagnosed, emergency surgery is required to anastate the vessel or release the compression.
Obstruction due to fat
- Rarely, attention should be paid to: multiple fractures, multiple soft tissue contusions.
- Threat of stun or shock:
- Conjunctival hemorrhage of eyes and skin
- Shortness of breath
- PCO2 high blood
- There is fat in the urine
- Urgent care is needed because of the high mortality rate.
The principles of treatment
First aid and first aid:
- Requires temporary immobilization and shock protection. In adults, up to 1 liter of blood can be lost through the fracture site. Poor immobilization can cause additional pain and possibly life-threatening shock. Therefore, it is necessary to prevent shock, need 1-2 liters of fluid and blood transfusion if available, then check if it is well immobilized before transporting it to the actual treatment place.
- If the fracture is scratched or has a large wound, a sterile dressing is required, strong intravenous antibiotics and anti-tetanus drugs are used.
- Solid femoral immobilization requires placing a brace beyond the pelvis, a convenient brace is the Thomas-Lardennois brace, which both immobilizes and pulls continuously lightly and quickly immobilizes it, especially in the case of a series of injuries. . In Vietnam, you can use bamboo and wooden braces. The brace must be large (10 cm) and thick (1 cm). Two or three splints can be used, usually two are used: 1 placed externally from the armpit to beyond the outer ankle; 1 brace at groin to medial ankle.
- True treatment: because the femur is large and strong, there are many strong muscles attached, so even with good manipulation, it cannot be fixed well in the powder, it is easy to move secondary. Currently, orthopedic treatments are mainly applied to children < 15 years old, the rest need surgery.
- Orthopedic method:
- Powder Bundle: only applied to children, the cases of multiple fractures with little displacement, non-displaced fractures, interlaced fractures. In addition, in the context of our country where there are not enough sterile conditions, tools and economics, this is the only method. After two months, when the bone has healed, it can be given on the powder for another 1-2 months. After opening the cast, the patient learns to walk with crutches, and gradually the quadriceps, hip and knee muscles will recover from 6 months to a year.
- Continuously pulling dumbbells through nails: usually applied to children (without surgery), the elderly, broken open, fracture, pathological fracture, poor general condition or pulling while waiting for surgery. The pull is performed mediated by a hook with # dumbbells 1/10 - 1/7 of body weight, pulling on the femoral shaft. It is possible to pierce the nail through the anterior tibial tubercle to pull in the case of fracture of the lower third, the inconvenience is to stretch the joint ligament. Or pull the bone through the condyle of the femur, allowing direct traction on the femur, without fear of stretching the knee ligament but inconveniently hindering bone fusion later. Large nails (Steimann 4 mm) are required. Should be pulled on Braun frame, knees slightly bent, feet 90o. The thighs should be kept behind to avoid excessive stretching. During the pulling period, daily clinical examination and weekly X-ray should be performed to adjust the weights pulled, starting to reduce weight gradually from week 8 and after 6 weeks can do pelvic-back-leg casts. During weightlifting, it is necessary to exercise the quadriceps muscles and joints to avoid complications after the bone has healed.
- Surgical treatment: is the most effective and active treatment available today.
- Intramedullary nailing: applied to fractures of the femoral body, preferably the middle 2/4 segment, applicable in all cases of transverse, diagonal, multi-fragment, and 2-focal fractures. Intramedullary nailing is considered the best method at present. Thanks to the bright curtain, the nail is not opened and the root canal is drilled wide. In order to prevent rotation of the distal fracture, the pin is reinforced across the bone. In the case of a low fracture line in the middle and lower thirds, intramedullary nailing with a transverse pin upstream from the lower femoral head can be performed. For fractures, it is possible to not need to drill the canal, just to arrange the bone in a straight line, people pull continuously for 2-3 weeks until there is a can to prevent rotation.
- Combining bones with a screw brace:
- The advantage is to completely straighten the broken bone and exercise early.
- Defect:
- Slow bone healing
- Limitation of muscle movements due to dissection during surgery
- Infection.
- Combination of bone screws is often applied in cases of fractures near the ends of bones.
- External fixation: applied in open fractures with soft tissue damage and neurovascular injury.
Preventive
Propaganda and education in the community about traffic and labor laws.
It is necessary to educate the community on local first aid and good immobilization of fracture cases to limit complications in fracture and shock.
For primary health care facilities, it is necessary to diagnose early, treat properly and transfer to specialized medical care for early treatment to minimize complications due to femoral shaft fractures.
Educate patients on rehabilitation exercises after treatment.
BREAKING BOTTOM LINES OF ALTERNATIVES
Outline
Fractures of the shin bone are cases of fracture of the tibial shaft from below the condyle to above the medial ankle, with or without fracture of the fibula from the neck to above the lateral ankle.
Frequency
Fractures of the shin bone are quite common, accounting for about 20% of total fractures and occur more frequently in men than in women.
Reason
There are two main mechanisms:
- Direct mechanism:
- Usually due to traffic accidents, labor accidents, due to heavy objects. Fracture occurs at any position depending on the place of impact, prone to open fractures from the outside in with heavy contamination.
- In addition to the above causes, sports accidents that break the tibia are characteristic of football.
- Indirect mechanism:
- For example, fractures caused by entrapment of the leg causing flexion of the lower leg are often cross, torsional, where the bone structure is weak (the junction of the middle and lower thirds). The fibula can break as high as the neck of the bone. The sharp-pointed socket can easily puncture the skin and cause an open fracture, risking damage to the lateral popliteal nerve.
Some notable anatomical elements
Interosseous membrane: strong, limiting the displacement of two bones.
The anterior and medial margins of the tibia lying close to the skin are not protected by muscles, the outer surface is covered by the extensor muscles but also fragile and while the posterior tibial surface is protected by the flexor muscle, and the force of this muscle mass is strong. 4 times the extensor muscle mass. At the top
distal to the tibia the muscles have transformed into tendons both anteriorly and posteriorly, the soft tissue that protects the fragile bone.
About circulation: there are three systems of bone nourishment (system in the canal, medulla oblongata and periosteum). The main artery feeding the tibia is a feeding artery that separates from the posterior tibial artery, passes through the bony feeding hole on the posterior surface, at the junction of the upper and middle thirds, into the canal to connect with the bulbar vasculature (Note Note: The feeding artery is vulnerable to fractures in this area).
Clinical symptoms
Closed fracture with displacement
– If you come early
Sharp pain in the broken area, the patient could not stand up.
Displacement is clearly seen with short limbs, lateral rotation of the foot, and posterior flexion.
Palpate the broken bone head under the skin on the medial side of the lower leg. Palpation also revealed sharp pain and the crunch of broken bones.
- If you're late
Often the leg is swollen a lot, it is difficult to detect symptoms such as sharp pain and broken bones. It is important here to pay attention to complications of compression of the posterior popliteal or tibial vessels cavity compression. Therefore, it is necessary to carefully examine the pulse in the instep, evaluate the degree of leg edema, and examine the sensation and movement of the toes. Urticarial nodules may appear, indicating an exacerbation of compartment compression complications. Examination should determine the ankle injury, fracture of the fibula neck, damage to the ligaments of the knee joint.
Fracture with little displacement
In adults, although there is little obvious deformity, a sharp pain point and slight protrusion of the fracture head may be seen.
In children, the type of fresh branch fracture is difficult to determine.
Complications of shin splints
Traumatic shock: rare in closed fracturecommon in open fractures. Broken bones in many pieces, crushed soft parts.
Cavity compression: accounting for 65% in body cavity compressions, usually occurs for upper third of tibia, multi-fragmentation, torsion fracture.
Vascular occlusion due to fat: common in cases of multiple fractures, soft tissue damage, early detection is required to save the patient. Watch out for these symptoms:
- Drowsiness (excluding traumatic brain injury)
- Eye conjunctival hemorrhage
- Hemorrhage in chest wall, armpit
- There are fat cells in the urine. Need emergency treatment with:
- Oxygen (6 liters/minute)
- Depersolone
- Heparin
- Lasix.
Infection: common in open fractures, rate inflammation of the bone quite high 12 – 30% (Cho Ray Hospital); 8.5% Allgoewer (Switzerland). Need good filtering, high dose antibiotics properly to limit infection.
Biến chứng vết thương da hở do xương chày nằm sát da và gập góc ra sau. Liệt thần kinh mác chung trong gãy cổ xương mác.
Nutritional disorders manifest early, appear blisters with fluid and blood. Late disorders after cast removal often see swollen feet, dry skin, pain. As a precaution, early mobilization and antithrombotic therapy should be exercised in patients with prolonged bed rest.
Joint prosthesis is a late complication, usually due to local causes such as:
- Three-piece fracture, the blood vessel does not nourish enough of the middle piece
- The fast healing of the fibula interferes with the healing of the tibia or because the fibula does not break.
Can bad, displaced:
- Tibia axis deviation > 20o the shaft needs to be adjusted.
- Bad hunchback in young people can be operated on due to cosmetic problems.
The principles of treatment
Treatment of shin fractures focuses on the treatment of tibia fractures. Even if the fibula is displaced, it does not affect the function of the lower leg. If treated early, the manipulation is relatively easy because there is not much swelling, there is little hematoma, and the muscles have not contracted much. If left late, there is a lot of swelling at the site, blisters can be seen, and the muscles are pulled strongly, so it will be difficult to straighten even in surgery.
Treatment goals include: creating good bone without shortening, not rotating, not stiffening the knee and ankle joints.
Bundle of dough
Applicable in the following cases:
- Fractures with no deviation or slight displacement regardless of the type of fracture (horizontal, diagonal, torsion) are fixed immediately. Thigh - leg - foot powder with longitudinal incision, bundled with the knee slightly flexed the foot 90o.
- After 7-10 days, when the swelling has decreased, you can wrap more dough in a circle or change another dough if the dough is too loose. During the bunion, instruct the patient to practice leg elevation, adduction, and abduction. After 3 weeks, gradually put on crutches and legs to avoid nutritional disorders. The dough keeps for 8-10 weeks.
- Fractures with a lot of displacement: Anesthetize the fracture and straighten it on a Boehler-type traction frame, pull with 7-14 kg weights, pull for 10-20 minutes. After pulling, check the length of the limb, the rotation, the need to correct the horizontal displacement, check the X-ray, then put a cast on the thigh - leg - foot or anterior cast, then check the X-ray after. If the X-ray examination shows little deviation, the patient should be placed on the leg elevated for 3-4 days. The powder keeps for 6-8 weeks, after 3 weeks for crutches.
According to Boehler, if the X-ray examination is still in the dough, it is recommended to stretch the weights on the dough for 3 weeks on the Braun frame.
According to A. Sarmiento, after pulling and straightening, put a cast on the thighs - shins - feet immediately, raise the legs for 3-5 days to avoid nutritional disorders, and let the patient practice lifting the legs up and down for 2 weeks. When relieving pain at the fracture, the thigh - leg - foot powder is converted into a functional powder under the knee so that the patient can exercise the knee joint and practice walking with crutches.
Functional powder keeps 8 - 12 weeks. This powder is often applied to the case of low fractures of the two bones of the lower leg.
According to some authors, if the tibia is fractured diagonally, twisted, cast as above is often unstable and easily displaced secondary. Therefore, it is recommended to pierce the nail through the heel bone for about 3 weeks and then switch to a cast.
Weightlifting
Use a large Steimann or Kirschner nail through the calcaneus for continuous traction on the Braun truss. Pulling weights is indicated in cases of unstable fractures, fractures with a lot of displacement. Pulling weights will correct short stack displacement, external rotation and some horizontal displacement.
Dumbbells are usually 1/10 - 1/7 of your body weight and increase every hour thereafter. Pull weights until clinically visible then switch to cast to shorten bed time.
Surgery
- Point:
Cases of twisted and twisted diagonal fractures that do not enter, suspected by software insertion
Two-stage fracture with long middle segment, complex fracture
Simple fracture of tibia in adults.
- Method
Intramedullary nailing: indicated in fractures of the middle third or the lower third of the tibia or in cases of fractures caused by direct mechanism of extensive bruising. Not indicated in upper 1/3 fracture. The technique can be closed or open. Nailing can use nails with pins to prevent rotational displacement, so the indication can be extended even to cases of upper third-high fracture.
Combination of screw splint: applied in cases of twisted cross fracture with 3rd piece, multi-fragment fracture, high fracture of tibia.
External fixation: applied in cases of complicated fractures or fractures with many soft tissue injuries, grade II and III open fractures.
Intramedullary nails and screws should be removed after one year. External fixation should be removed when the socket is broken.
Physical therapy
In addition to elevating the legs to prevent post-operative edema, an exercise program is required as soon as the patient is awake. Need to exercise the muscles gently and without pain.
The advantage of surgery is that the bone heals according to the wishes of the treatment, the joints are not stiff, and the patient quickly returns to normal activities. However, the risk of infection during surgery is still high due to the lack of sterility (10-25%). In addition, complications of splinting and splinting may also occur.
Preventive
Propaganda and education in the community about traffic and labor laws.
It is necessary to educate the community on local first aid and good immobilization of fractures in cases of fractures to limit complications in fractures.
For primary health care facilities, it is necessary to diagnose early, treat properly and transfer to a specialized medical level for early treatment to minimize complications due to two shin fractures.
Instruct patients to practice rehabilitation after treatment.





bài viết rất hay ạ