Table of contents [hide]
GENERAL SITUATION
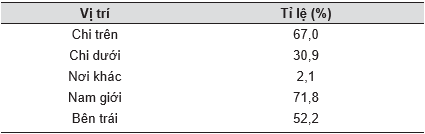
In Children's Hospital 1, Ho Chi Minh City, every year there are nearly 2,100 injuries requiring hospitalization, of which 68% are fracture. The distribution ratio is as follows:
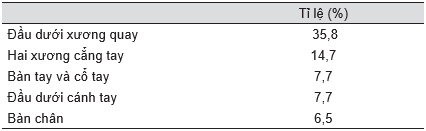
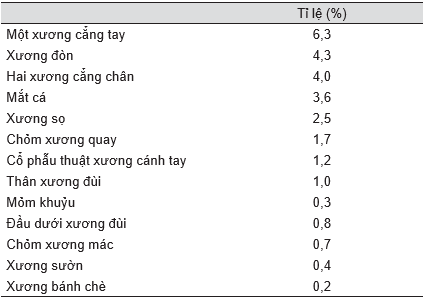
Table 8.1. Fracture distribution rate
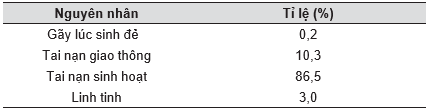
About the cause:
The age group with the most fractures is between 6 and 10 years old.
Statistics of Worlock in 1986 with 923 cases of fractures in children showed that:
In Western Europe, the age of children with multiple fractures is 5-12 years old.
The types of old fractures that go to the hospital to ask for orthopedic correction are 5-9% for general fractures.
The above situation shows that it is necessary to attach importance to the prevention of traffic accidents, jokes and falls at home and especially at school.
OUTLINE
Anatomically, this article does not address the types of trauma to the craniofacial and maxillofacial, nor does it mention the types of dislocations (other articles).
As in adults, there are two types of fractures in children:
- Fracture due to trauma
- Pathological fracture (inflammation of the bone, bone tumor,…).
The following refers only to traumatic fractures.
Because of the time scope, it must be limited as above, but when it comes to managing a fracture, both children and adults must systematically examine the patient and manage sequentially, prioritizing internal injuries. organ can affect the patient's life, should not focus too much on the fracture and delay the general management.
The differences between adult and child bones are:
- Presence and activity of synaptic cartilage
- The artificial bone at the end of the bone
- The role of horizontal bone enlargement of children's periosteum
- The overall development of the body is faster as the baby is younger.
The above points stabilize gradually and are quite similar to adults when they are 12 years old or older. In general, wounds and fractures in children heal faster than in adults.
According to Zanoli, the unit of time heal bones In adults, it's months, in children, day by day, femur fractures in infants heal from 14 to 21 days, the can is very large but the shape returns very quickly after that. The ability to self-correct the fracture is a great feature to know in the treatment of fractures in children.
Self-adjusting deformation mechanism:
Deformities (if any) that persist after the fracture has healed can be of four types:
- short
- Lateral displacement (ladder type)
- Corner Folding
- External or internal rotation (pronation towards forearm).
When two fractures overlap and heal in such a shortened position (no more than 2 cm), some time after the fracture, the bone will lengthen to compensate and equal to the healthy limb. This mechanism is due to stimulation by cyclic changes in the fracture that affect the synaptic disc activity (according to Trueta and many other authors).
According to Pauwels, growth stimulation at the synaptic cartilaginous surface is irregular, concentrated in new lines of force. According to the above mechanism, the "staircase" deformation gradually disappears. After 1-2 years of shooting X-ray examination will no longer recognize where the bone is broken.
Cornering distortion is also self-correcting. It is important to know that even with a natural self-regulating mechanism, the physician should not be negligent and must correct the angulation. Angle deformity located in the plane of motion of the joint (flexion, extension, etc.) has a very good outcome, but if the angular displacement is not in the plane of motion, the self-correction is worse.
Rotational displacement that cannot be self-corrected requires the physician to correct this displacement, and in many cases, it has to be corrected by chiropractic surgery.
CLINICAL
Fractures in children can occur from birth (difficulty birth) and more often when the baby learns to walk, at most between the ages of 6 and 10.
The can is very large: sometimes makes inexperienced people think it is a bone tumor (clavicle, humerus, ...) usually disappears a few months later.
Fractures make the newborn unable to move (thought to be paralysed), sometimes it has to be distinguished from other forms of paralysis due to difficult birth trauma, damage to the brachial plexus such as at the C5-C6 roots (syndromic syndrome). Duchenne-Erb). A close examination reveals a can, thereby confirming the diagnosis of a fracture.
In neonates, fractures usually heal within 21 days, sometimes the femur flexes nearly 90 degreeso which X-ray examination 2 months later did not recognize the old fracture thanks to the self-correcting mechanism.
Very rare types of fractures in children are: fractures of the spine, calcaneus, patella, etc.
When a broken forearm or lower leg bone is examined, check (clinically and radiographically) whether the remaining bone is fractured or dislocated (eg, Monteggia,…).
X-RAY
Many doctors are confused when watching X-ray films of children's skeleton because the synovial cartilage is still abundant and not contrasted. In addition, there are many artificial bones that develop with age that are difficult to remember, so the solution is:
- X-rays show the injured side with the healthy side to compare abnormalities in areas with many synovial cartilages. The child's size is small, so it is usually easy and inexpensive to capture both the sick and the healthy side on the same film.
- Both planes (straight and oblique) should be taken as in adults to show all fractures and displacements.
A "green tree" fracture (fresh branch fracture) is a fracture on one side of the cortical bone, it is necessary to take both planes to clearly detect this particular type of fracture.
Cần xem kỹ trẻ em có nhiều xương phụ (accessory bone) dễ lầm tưởng là gãy xương (bên trong xương thuyền bàn chân, xương hạt đậu,…).
Must detect for good management of synovial detachment in the area near the cervical crest, for urgent manipulation.
There are fractures that only crack the bone, 7-10 days after seeing the bone can, many people mistakenly think it is a bone tumor, this can disappear gradually 1-2 months later. Other types of cage fractures also cause the same condition (radial, tibia, …).
THE PRINCIPLES OF TREATMENT
- First aid: must ensure pain resistance, put a good anti-pain brace before moving like in adults
- Because canes grow very quickly, they must be straightened very early: "in the night"
- Correction is not perfect, does not need to be as accurate as in adults thanks to self-correcting mechanisms, but must correct all rotational displacement.
- Time motionless shorter than in adults
- Very little need for physical therapy intervention
- Most are treated conservatively with very little surgery.
TECHNICAL ISSUES
Điều trị bảo tồn là nắn và cast hoặc kéo tạ ít lâu rồi bó bột. Kỹ thuật nắn đòi hỏi phải chuẩn bị gây mê và gây tê để tránh sự giãy giụa của bệnh nhân vì sợ, đau,… như thế bó bột mới được tốt hơn. Khi cần kéo tạ thì kỹ thuật thường dùng là kéo da (không xuyên kim qua xương như ở người lớn) bằng băng dính dán sát vào da cẳng chân, cẳng tay. Trọng lượng kéo có thể tới 3 kg. Mục đích việc kéo tạ là chờ khi xương có can lâm sàng sẽ chuyển sang bó bột hoặc để săn sóc vết thương trong broken open. In rare cases, a Kirschner needle can be inserted through the elbow to straighten fractures on the two condyles of the humerus with significant displacement.
Fresh branch fractures must be straightened completely and cast immobilized like other fractures.
Bundle of dough
The cast must be placed over the two joints above and below the fracture as in adults, but the immobilization period is shorter. The monitoring of complications after casting must be very careful to detect complications of sub-cast compression as soon as possible, to prevent circulatory disorders, sometimes leading to Volkmann syndrome or other complications. cavity compression other.
Cases of cage fractures, fractures can be splinted, but because they are children or naughty, it is better to give a thin, safe cast than to put a brace.
Surgery
Indications for surgery include:
- Piece of bone in joint socket
- Displaced multiple lateral condylar fractures of the humerus
- Fracture of the rotator cuff at an angle > 45o (surgery to correct it, not throw it away like some cases in adults)
- Fracture of femoral neck
- Gãy xương bánh chè
- Fracture of the talus
- Some fractures of the synaptic cartilage cannot be preserved
- Some fractures of the two forearm bones have a lot of displacement
- Old fractures and old dislocations have counter-functional deformation.
Physical therapy
The main thing is to let the baby naturally not massage even a gentle massage, especially in the elbow area, doing so can easily cause permanent stiffness.
In children, stiffness after cast removal is temporary and does not require intervention.
PROTECTION, COMPLAINTS
Except for some medical conditions, closed fracture trauma without bone healing (pseudomembrane) is very rare in children.
There are four cases of bone failure:
- It was supposed to be surgery but not surgery
- It should have been an operation without surgery but surgery
- Pathological fracture (congenital prosthetic joint) that is thought to be a traumatic fracture
- Open fractures that lose a lot of bone (fire wounds, etc.).
Complications of BACKGROUND IN CHILDREN
Infection
Physicians must pay attention to two issues:
- Tetanus
- How to use antibiotics.
The details of management are discussed in a separate article, but surgically:
- Resection is essential if there is an open fracture.
- Note three types of infections:
- Golden Stabilizer
- Clostridium tetani (Tetanus)
- Clostridium perfrigens (vapor gangrene).
Blood vessel damage
Symptoms of blood vessel damage: below the fracture site
- There is no pulse or it is present but very weak compared to the healthy side
- Cold skin
- Poor capillary and venous activity.
Injury location: near the fracture, dislocation, often found in the elbow, hip joint, and hip region.
Diagnosis needs to be confirmed urgently, accurately, by angiography, digital background scan (DSA), whenever it is difficult to catch pulse, large swelling hematoma, unexplained drop in blood pressure.
In case there is no condition to do DSA but the injury time is nearly 6 hours, exploratory surgery is required for timely treatment; especially pay attention to cases where the symptoms only have "weaker pulse" than the healthy side or the pulse is weaker than a few minutes ago! This is a feature of many cases where the injury does not completely break the blood vessel, but only bruises the intima, leading to thrombosis (thombosis), especially in the popliteal region of children.
Immediately intervene if the pulse still does not return, despite the correction and immobilization of the fracture; should not be based on the "warm feet" sign. Many scientific reports have identified 90% to be saved from amputation if circulation is reestablished before 6 h. With anemia, children's nervous and skeletal muscle tissue is more susceptible to damage than adults, the risk is higher if treated more than 6 hours after the accident.
Arterial lesions must be sutured, but venous lesions are currently not agreed upon on how to manage.
In terms of surgery, autologous veins should be used for transplantation if necessary; synthetic materials should not be used; Bones can be shortened to connect blood vessels (the length of children's bones can be adjusted later). Broken bones are immobilized first; vascular treatment follows.
Particularly in children, success in limb jointing and preservation is not necessarily successful in terms of Rehabilitation, because later disorders can occur at multiple sites, infection, damage to the synaptic cartilage.
Must take care of and monitor the child until adulthood.
Peripheral nerve damage:
- Tổn thương trực tiếp do mảnh gãy: thần kinh quay, thần kinh tọa
- Injury to the small branch: interstitial nerve - forearm bone due to fragmentation on the two condyles of the humerus in children.
- Tổn thương gián tiếp do rối loạn phát triển sụn tiếp hợp: liệt muộn thần kinh trụ do biến dạng valgus ở khuỷu nhiều năm sau gãy lồi – cầu – ngoài đầu dưới xương cánh tay trẻ em.
Cần lưu ý các ca gãy kín có triệu chứng liệt thần kinh quay ở cánh tay và khuỷu thường phục hồi trong vòng 2 tháng; quá 2 tháng không phục hồi hoạt động thần kinh, phải giải quyết bằng phẫu thuật (gỡ chèn, gỡ mô xơ, khâu nối thần kinh).
Compartment syndrome:
In general, compartment compression in children has the same characteristics and symptoms as adults, can occur in the forearm (Volkmann syndrome), hands, legs, feet, due to contusion trauma, accidents vehicle, sport, with and without fracture; only fasciotomy should be done; If the fibula is cut, later the ankle is deviated, valgus deformity.
- Tissue pressure 30 mmHg: 6-8 hours later, the skeletal muscle tissue is caseation
- Tissue pressure 40 mm/Hg: urgent decompression surgery
- Tissue pressure 50 mm/Hg: complete loss of nerve conduction.
In terms of timing, the prognosis is good if the patient is decompressed within 12 hours of the accident.
Vascular occlusion due to fat:
Usually occurs with long bone fractures; Drummond said 0.5% out of 1,800 children had fractures of the pelvis and femur, compared with 5% for similar cases in adults. Older children are more often affected, within 2-3 days after the accident.
Doctors must monitor and pay attention to cases of shortness of breath, children struggling, lethargy; need for oxygen (above 7 L/min) and special resuscitation.
Deep vein occlusion due to thrombosis
Rarely in children; symptoms as in adults.
Abdominal syndrome due to cast
Abdominal bloating with vomiting:
Classically, this syndrome occurs due to a large cast that compresses the abdomen. This syndrome is seen today even without a cast; Abdominal syndrome also occurs after spinal surgery, Harrington brace to correct scoliosis, and Scheuermann's disease (teenage kyphosis).
Causes of abdominal syndrome: D3 segment of the duodenum is compressed by the superior mesenteric artery.
High blood pressure from lifting weights:
Author Hamdan noted that 68% children who were lifting weights had high blood pressure and had to adjust the pull.
Hypercalcemia due to immobility:
Urinary calcium levels increase after 4 weeks of immobilization, especially in older children.
Patient loss of appetite, vomiting, muscle weakness, irritability; require a low calcium diet and monitor serum calcium for 6 weeks after initial symptoms.
Sudeck atrophy:
Pain, burning sensation burn, poor rehabilitation, lasting up to 4 months, often accompanied by psychotic symptoms, but milder in adults.
Loose ligaments
Usually occurs in the back cervical spine, between the spines (C4-5, C5-6, C6-7).
Routine X-ray knee joint to test the wire front cross (tibular spine) whenever there is an injury to the thigh or lower leg.
Injury to the Y acetabulum cartilage: Rare, can be seen in children under 10 years of age
Sequelae: shallow acetabulum + semidislocation of femoral head.
Bone growth in muscle
- Reason:
- Rough physical therapy
- Massage the elbow area.
- Treatment: avoid massaging the elbow fracture, exercise slowly, let the baby live naturally.
Bad luck
Often seen after fracture, the two bones of the forearm are displaced a lot, due to poor adjustment. The two forearm bones are firmly adhered at the fracture site (X deformity).
Surgical treatment, at least 1 year later, detailed dissection, two separate incisions.
Late corner bend
Damage due to fracture in the metaphysis, damage to the outside of the superior tibial synovial cartilage; must wait 18-24 months before deciding to have osteotomy.
Prosthetic joint
Rare in children, but can occur due to improper manipulation and immobilization, surgical infection.
It should be distinguished from congenital prosthesis, which is very difficult to treat due to Recklinghausen's disease.
Fracture recurrence
Usually occurs in young children, hyperactive, frequent falls, sometimes the old fracture breaks again 12 months later.
It should be differentiated from other congenital diseases such as osteogenesis imperfecta.
Synaptic cartilage dysfunction (physis)
Children's femur fractures usually add 1 cm (0.4 – 1.7 cm) in length at any age; The ipsilateral tibia also increased by an average of 0.29 cm (Shapiro).
The above phenomenon occurred up to 18 months after the fracture accident; 9% continued to slightly prolong the remainder of synaptic activity, especially at ages 4–8 years (Staheli).
For this reason, when treating a femur fracture, it is advisable to overlap the fracture by approximately 1 cm.
The current topical problem is the phenomenon of partial fusion of the synaptic cartilage (previous synovial ossification, growth arrest) after trauma; It is necessary to accurately diagnose (by MRI, CT-scan) the position of the bone bridge to properly dissect the adhesion.
ACCIDENT PREVENTION
Broken bones happen at any age, so from midwives to parents and teachers, everyone is responsible.
Boys must be given extra attention, especially at school age, in all activities near home and around school. There are twice as many fractures in the upper limbs than in the lower limbs. This speaks to the important issue that the intensity of the children's running and jumping must be restrained by the adults, because the self-protective reflexes of the upper limbs are not good, but the mischief is too much and falls often.
For traffic accidents often caused by careless drivers, children should be dressed in bright colors so that the driver can easily see and avoid them.




