Table of contents [hide]
DEFINE
Osteoarthritis is a degenerative degenerative disease of the joints, first manifested in the articular cartilage, then there are changes in the joint surface and the formation of bone spurs, finally leading to joint deformity. Mild synovitis is a secondary manifestation of degenerative changes in articular cartilage.
Epidemiology
Osteoarthritis is the most common disease in the joints, in the elderly, both men and women. About 50% people over 65 have pictures X-ray Acute degenerative joint disease, in people over 75 years of age with X-ray images of degeneration in at least one joint.
Most patients with osteoarthritis have no clinical symptoms, only 5 - 15% patients have clinical symptoms, then it is called degenerative joint disease.
Occupations are associated with higher rates of osteoarthritis, porters and miners have higher rates of disease than those who do light work.
Between the ages of 45 and 55, the incidence is equal in men and women, but after the age of 55 the disease is more common in women than in men.
PHARMACOLOGY
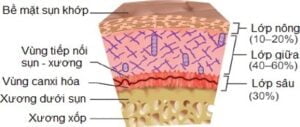
Normal cartilage structure
The cartilage structure consists of three main regions: the surface area is mainly composed of chondrocytes that protect the middle and deep regions of the cartilage. The main components of cartilage include water, proteoglycan, collagen fibers.
Proteoglycans It is abundant in the medial region of articular cartilage, containing a protein core and adjacent glycosaminoglycan chains and mainly chondroitin sulfate and keratan sulfate. The proteoglycan bodies bind to hyaluronic acid, other glycosaminoglycans and proteins associated with this structure to ensure the stability and stability of the cartilage.
Collagen fibers gather in the deep areas of articular cartilage, which are also important structural and functional components of cartilage. The main collagen in cartilage, articular cartilage is collagen type II, in addition, there are collagen types I, IX and XI.
Pathogenesis of osteoarthritis
Many theories explain cartilage degeneration in osteoarthritis. But mainly the mechanistic theory when there is a mechanical overload that changes the metabolism of the chondrocytes, forming proteolytic enzymes that break down the basic substances of the cartilage. The first pathological phenomenon is small fractures of various sizes; then cause degeneration and gradual loss of articular cartilage, change the structure of joints and form bone spurs.
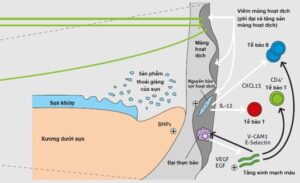
In the early stages, chondrocytes show hypertrophy, increased secretion of cytokines such as Interleukin I (IL-1); element caseation Tumor (TNFα) and other growth factors, enzymes that digest basic substances such as collagenases, gelatinase, stromeolysin, other enzymes such as lysosyme and cathepsin. IL-1 and TNFα induce cartilage degeneration by stimulating the secretion of enzymes that destroy collagen and proteoglycans, and by inhibiting synthesis of cartilage matrix proteins.
stick-like
The enzymes collagenases, gelatinase, and stromeolysin are inhibited by a protein of small molecular weight, called a metaloproteinase reorganization inhibitor. The balance between stimulants and inhibitors of enzyme activity ensures normal cartilage metabolism. When increased enzyme activity stimulating factor leads to cartilage degeneration. The process of osteoarthritis is uncontrolled, because when there is a change in cartilage structure, the mechanical impact on the joint also changes, leading to heavier overloads, releasing more degenerative enzymes and continuing as Thus, the degradation process continues.
Risk factor
- Trauma and micro-trauma have an important role in changing the cartilage surface, major injuries cause fracture, dislocation accompanied by cartilage damage or redistribution of pressure on the articular cartilage surface.
- Endocrine and metabolic factors: acromegaly, hypothyroidism, postmenopausal women
- Birth defects, loose joints
- Arthritis acute or chronic bacterial infections (purulent arthritis, tuberculosis)
- Arthritis due to chronic joint diseases (rheumatoid arthritis, ...)
- Anemia, bone necrosis
- Bone dystrophy
- Nutritional disorders after neurological diseases
- Blood clotting disorders (hemophylia), hemangiomas
Histopathology
Overall
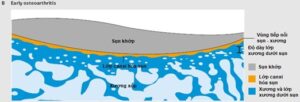
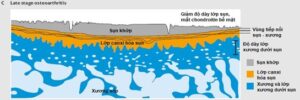
The cartilage surface is not smooth, loses its shine, has cracks, ulcers on the cartilage surface, exposes the subchondral bone, thickens the subchondral bone layer and has bone spurs at the edge of the articular cartilage.

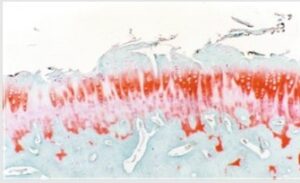
Microscopic
In the early stage, small fibers are seen, the cartilage surface is uneven, the cartilage layer is thinned, corresponding to the macroscopic change, in the very early stage, inflammatory cells can be seen but only for a short time, the image Inflammatory lesions are uncommon in osteoarthritis.
Injury to the synovial membrane is a secondary manifestation and often later changes in fibrosis of the synovial membrane and joint capsule, sometimes with synovial effusion secondary to small fragments of cartilage that become dislodged into small foreign bodies in the joint. Irritated joints resembling microcrystalline arthritis.
CLINICAL
The typical clinical presentation of osteoarthritis is often seen in middle-aged or elderly patients. Presents pain, stiffness in or around the joint, accompanied by limited joint movement. Pain of slow onset, moderate or mild pain. Pain increases with movement, walking, carrying heavy loads, pain decreases or disappears with rest. Pain at rest or at night is often associated with secondary synovitis.
The mechanism of pain in osteoarthritis has many factors such as inflammation around the fracture site or subchondral bone breakdown, stimulation of nerve endings by bone spurs, paraarticular muscle spasticity, bone pain due to increased current. blood pressure and increased bone pressure, synovitis due to increased synthesis and release of prostaglandins, leucotrienes and cytokines.
- Morning stiffness is also common in osteoarthritis, but the duration of morning stiffness is short, less than 30 minutes, different from rheumatoid arthritis. Stiffness after rest or inactivity is common, which goes away after a few minutes.
- Many patients find that pain and stiffness often appear when the weather changes such as cold, rain, sunshine, etc. It may be due to the change in pressure in the joint that is related to the change in atmospheric pressure.
- Degenerative patient knee joint often feel pain and unsteadiness, pain increases when going down stairs or when bending the knee.
- Osteoarthritis patients often have pain in the groin area, sometimes spreading down the back of the thigh to the knee joint.
- Degenerate cervical spine, or the lumbar spine causes neck pain and low back pain, sometimes fractures can cause nerve root compression, causing nerve root damage syndrome: pain, muscle weakness, numbness.
- Physical examination: often detect symptoms in painful joints such as hypertrophy of the ends of bones, pain when examining the organization next to the joints or the attachment points of the joint capsule, ligaments, tendons.
- Limited joint movement due to bone spurs, uneven cartilage surface, or paraarticular muscle spasticity. Stuck in the joint when moving can be due to a rupture meniscus or detachment of cartilage fragments into the joint socket.
- The crackling sound when moving the joint is due to the uneven joint surface, this sign is seen in about 90% patients with knee osteoarthritis. About 50% patients with knee osteoarthritis have signs of ligament damage, bow-legged joint deformity, pain when moving due to joint capsule irritation, paraarticular muscle stiffness and inflammation around the bone spurs.
- Localized signs of inflammation include heat, swelling, and effusion in the joint socket
- Patients with multi-joint degeneration may have signs of distal arthritis, arthritis of the proximal knuckles of the hand
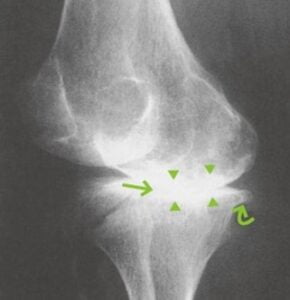
SUBCLINICAL
- Diagnosis of osteoarthritis is usually based on changes in the X-ray image of the joints. Typical X-ray symptoms are bone hypertrophy, bone spurs at the edge of the joint. Uneven joint space narrowing, dense subchondral bone. Joint space stenosis can be caused by thinning of the cartilage layer, or by calcification of cartilage in the area of bone spur growth.
- In the late stages, the appearance of cavities in the ends of bones, bone regeneration, changes in bone head shape, central bone defects, cortical collapse in the distal joint or sometimes in the knuckles near the hand are manifestations of multiple degeneration. joint.
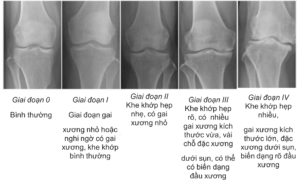
- In addition, for the knee joint, it is possible to classify the degree of degeneration based on X-ray according to the authors Kellgren and Lawrence.

DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
Diagnosis of osteoarthritis is usually based on history and physical examination. The results of routine tests are less variable. It is important to distinguish between two confusing situations.
- Differentiate osteoarthritis from patients presenting with arthritis
- Differentiate secondary osteoarthritis in patients who already have rheumatoid arthritis or other diseases related to osteoarthritis.
THE PRINCIPLES OF TREATMENT
General principles
- Relieve pain symptoms
- Maintain, or treat Rehabilitation of joints
- Avoid unwanted drug effects.
Therapeutic measures
1. Non-drug treatment
- Patient Instruction
- Support from family and society
- Treatment with physical therapy, exercises to support the cervical and lumbar spine
- Other supportive sports such as swimming (except breaststroke), cycling (high saddle, flat road).
2. Drug treatment
- Pain relievers such as acetaminophen are often used. Patients with unsuccessful acetaminophen therapy may be due to non-steroidal anti-inflammatory drugs unless contraindicated.
- Non-steroidal anti-inflammatory drugs: have both analgesic and anti-inflammatory effects. When using non-steroidal anti-inflammatory drugs to treat osteoarthritis often increases the risk of complications on the gastrointestinal tract (inflammation, ulceration, bleeding, ulcer perforation, kidney complications, ...).
- Glucosamine and chondrointin sulfate are effective in reducing the progression of moderate to severe osteoarthritis.
- Intra-articular corticosteroid injection to treat osteoarthritis with secondary effusion: has analgesic effect due to strong and rapid reduction of inflammation. Injection of joint socket needs to ensure absolute sterility.
- Injections of hyaluronic acid and platelet-rich plasma have been shown to reduce pain and improve function in patients with early knee osteoarthritis.
- Stem cells used in the treatment of degenerative joint diseases are mostly extracted from bone marrow, adipose tissue or peripheral blood. Intra-articular injection of stem cells is supported by many authors because both have positive effects on osteoarthritis patients after 1 year of follow-up. However, there is still a lack of evidence on safety and efficacy in degenerative disease at long-term follow-up.
3. Surgical treatment
- Patients with ineffective medical treatment or have a great impact on joint mobility can use surgical intervention. Currently, it is possible to operate many patients with early stage knee osteoarthritis by endoscopic surgery, cleaning, drilling to stimulate bone formation, endoscopic autologous bone cartilage grafting, autologous chondrocyte transplantation, copper cartilage grafting. type.
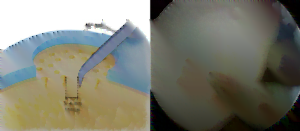
- The osteogenesis-stimulating arthroscopy method has the advantages of reducing pain and improving function, having the formation of both fibrocartilage and hyaline cartilage, and the technique is low-cost and quite simple. However, this technique can only be performed when the lesion area is small (less than 2 cm .).2), the effect begins to decrease after 18 months and is age dependent: less than 40 years of age the results are better.

- Endoscopic autologous cartilage grafting: is a technique to remove cartilage and bone blocks from a relatively unloaded area and graft into the area of cartilage defect. The advantage is to restore the cartilage form The disadvantage is that it causes damage to the bone cartilage area, there are few places to take it and this is a difficult technique.
- Autologous chondrocyte transplantation is a technique of culturing and proliferating chondrocytes, grafting back into the cartilage defect area below the periosteum. The advantage is the restoration of normal hyaline cartilage. Disadvantages need two surgeries and cost of cell culture.
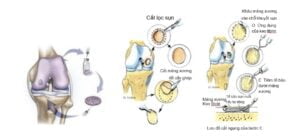
- Allogeneic cartilage grafting: is a one-stage surgery, especially indicated when the cartilage defect is > 2 cm2, diffuse subchondral bone edema. The results are good for patients with focal idiopathic cartilaginous lesions of the condyle. Disadvantages include: transplant rejection, infectious diseases. Poor outcome when both condylar cartilage and tibial plateau are > 10 cm2, chronic injury, old age, crooked knee. Cartilage grafting for patella has little research, osteoarthritis: failure 48%
- Cắt xương sửa trục nhằm thay đổi trục chịu lực chi dưới làm giảm chịu lực khoang gối đang bị tổn thương và giảm đau. Từ đó, làm chậm quá trình thoái hóa, kéo dài thời gian đến lúc cần thay khớp
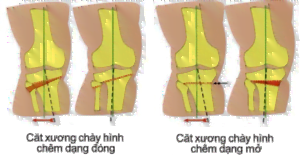
- This method has the advantage over knee replacement in preserving bone mass and structures in the joint. Indicated in single-compartment degeneration with internal or external deformity, usually in young patients as an alternative to joint replacement (wearing poly layer). However, the damage to articular cartilage could not be restored and it was difficult for later knee replacement surgery, so it gradually went down in history.
- Indications for artificial joint replacement surgery in late stage osteoarthritis. When the hip osteoarthritis is already in a severe stage, the patient has pain both at rest, at night or on X-ray film of the deformed femoral head. Or when damage to the knee joint reduces and loses mobility, causing pain that doesn't go away with any other treatment and care.
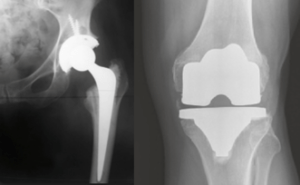
- Single-compartment knee replacement can be performed if the patient has indications: single-compartment degeneration, > 60 years of age, low mobility needs, not obesity, ROM > 90o, < 5o fold shrinkage < 10o Forehead plane deviation can be passively corrected. This method is suitable for young patients because of maximum soft tissue preservation, minimal bone resection, reliable in elderly, sedentary people.

ABSTRACT
Osteoarthritis is the most common degenerative joint disease. The disease manifests as pain and stiffness in or around the joint, accompanied by limited joint movement. The diagnosis of osteoarthritis is usually based on the history of the disease, physical examination, and changes in the X-ray of the joints.
Treatment of osteoarthritis includes non-pharmacological measures, drug therapy and surgical treatment.




