Table of contents
OUTLINE
Advances in medical technology allow doctors to diagnose and treat injuries that went unnoticed 20 years ago. For example, using a small camera lens to look inside the joint. With the help of this tool, today's surgeons are able to diagnose and treat a number of injuries and diseases. shoulder, of which a meniscus tear is treated with arthroscopy shoulder showed positive results with minimally invasive intervention.
The most common site of parietal cartilage damage is the inferior anterior capsule cartilage complex (84-97%) (also known as Bankart or Perthes lesions). Posterior shoulder instability occupies 5%. The multidirectional parietal cartilage lesions described by Neer and Foster in 1980 include anterior, posterior, and inferior instability.
Historically, treatment of shoulder instability in the past has often focused on limiting joint mobility, and anatomical restoration of torn meniscus is often not performed. The best examples of these reconstruction techniques include subscapular transfer (Magnuson-Stack), subscapular and capsule cross stitches (Putti-Platt), and craniosynostosis and tendon transfer (Bristow) -Latarjet). As surgeons have gained a better understanding of the functional anatomy of the shoulder, the treatment of shoulder instability has relied on restorative anatomy.
ANATOMY
Functional Anatomy
The shoulder joint plays an important role in connecting with other parts of the body such as shoulders and arms to support the movement and movement of people.
The shoulder joint is a multiaxial synovial joint. The shoulder joint is made up of the hemispherical humerus and the scapula. The humerus is located in a shallow joint in the shoulder blades called the socket. The humeral crest is usually much larger than the socket and a ring of soft fibrocartilage tissue about 4 mm thick called the parietal cartilage surrounds the joint to stabilize the joint. This filament deepens the socket up to 50% for a better fit of the humeral head, where the anteroposterior depth (9 mm) is deeper than the anteroposterior depth (5 mm). Saha has shown that the addition of alveolar rim cartilage increases the contact surface of the alveolar joint with the brachial crest to 75% longitudinally and 57% horizontally. Karzel et al., in biomechanical testing of cadaver shoulder samples, showed that the parietal cartilage affects the distribution of the contact area when a compressive load is applied to the shoulder at a 90-degree angle. °.
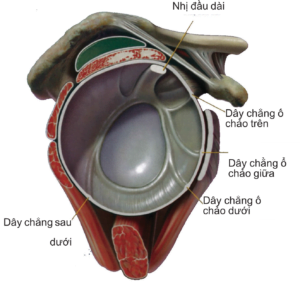
The articular capsule and ligaments of the shoulder, including the biceps tendon, are attached to and become part of the marginal cartilage, which attaches to the socket. The alveolar cartilage is the attachment point for several ligaments, such as the superior, medial, and inferior brachial ligaments. The superior lateral margin is the origin of the long head of the biceps tendon, while the lower margin is the partial origin of the long head of the triceps. The posterior and superior margins of the lateral alveolar cartilage provide attachment for the fibroarticular capsule, while the medial surface is in direct contact with the brachial crest and is demarcated by the synovial membrane. The superior and anterior superior portion of the alveolar margin cartilage adheres loosely to the alveolar rim, unlike the inferior attachment.
Injury surgery
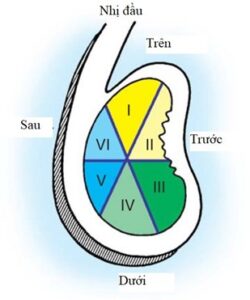
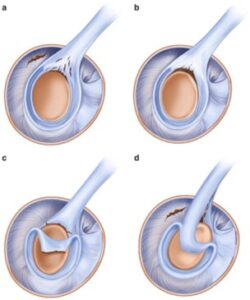
To assist in locating the parietal cartilage damage, the parietal cartilage was divided into six areas: (1) superior parietal cartilage, (2) anterior parietal cartilage above the medial alveolar groove, (3) anterior parietal cartilage in below the medial sulcus, (4) inferior parietal cartilage, (5) posterior inferior border cartilage, and (6) superior posterior border cartilage (Figure 2). Several mechanisms of injury have been identified including compression, pulling, pulling, tearing, and chronic degenerative changes. Tear pattern can be identified through arthroscopic imaging, similar to tear meniscus at the pillow. Common types of tears include flap tears, book loops, inseparable tears, degeneration, and SLAP (Superior Labrum from Anterior to Posterior) tears. Lesions located on the equator of the socket (a line between the 3 o'clock and 9 o'clock positions on the socket) are usually associated with rotator cuff tear or biceps tendon disease. Lesions located below the equator, most commonly anterior and posterior, are detached, non-separate lesions, which are highly suggestive of shoulder instability.
A SLAP lesion is an anterior to posterior tear of the superior border cartilage. Occurrence in throwers may be due to the secure posterior attachment of the inferior brachial cruciate ligament altering the posterior superior contact point and increasing the tearing force on the superior parietal cartilage. Injury to the SLAP increases the strain on the anterior band of the inferior brachial cruciate ligament and thereby affects shoulder stability.
REASON
There are two main causes of shoulder cartilage tear. These are: muscle strain and postural injury.
Muscle tension
Sự căng trương lực cơ tự phát kéo dài là một sự co cơ chống đỡ không đẳng trương
̣ (muscle contraction without significant reduction in muscle fiber length). Since there is no shortening of the muscle fibers, there is no joint change in the body, no movement occurs, but there is an increase in force from the short fibers which changes all the chemical, electrical as well as electrical components. is converted to the circuit.
Heavy exercise is also a cause of muscle pain, which can persist for several hours after rest due to disruption of the system by prolonged muscle contraction, especially in sports. This is referred to as a reflex mechanism, in which there is tension in the golgi apparatus to counteract muscle contraction.
Metabolism products during muscle contraction such as "P-factors", potassium, and lactic acid also become factors that stimulate local pain receptors.
Some excessive muscle contraction will cause microscopic tearing of muscle fibers, causing edema, inflammation of the periosteum of the muscles attached to the skeletal muscle and subperiosteal tissues, leading to pain and increased pain sensation in people with injury
Posture injury
In daily activities, there are many activities that are subject to excessive shoulder posture such as: sitting posture at a computer desk, prolonged standing posture (receptionist professions, marketing, etc.) , sports that use a lot of force in the shoulders and arms (badminton, tennis, volleyball, basketball, ...) These postures lasting for a long time are one of the causes of torn meniscus. shoulder.
SYMPTOM
Physical symptoms
Medical history may raise suspicion of shoulder instability. The patient's age, occupation, employment status, activity level, dominant hand, and other medical problems are helpful in categorizing the nature of the instability. Certain circumstances, such as work-related injuries or disputes, can affect a patient's perception of their disability and their expectations. on recovery and adherence to treatment.
Look for specific complaints. For example, a patient may point out that the arm is "helpless" during a fight for the ball. This symptom may be related to a traumatic subluxation and the presence of a Bankart lesion. Another example is a patient with a history of getting stuck and then waking up with a feeling that the joint is “in the wrong place”. This condition indicates a posterior dislocation caused by uncontrolled internal rotation over the weaker external rotator cuff muscles of the shoulder.
If pain is the primary factor in the patient's complaint, what activity is causing the pain? Ask athletes about the type of sport, the position played, and the duration, frequency, and level of participation. For example, throwers, swimmers, or tennis players may develop excessive laxity as a result of their shoulder being subjected to repeated minor trauma. The result is a recurring shoulder subluxation, which can produce a feeling of "looseness" or "slipping" during activity. In addition, as noted previously, secondary “hard to escape” conflicts can occur because anterior instability reduces the space below the apex, causing pain during overhead activity. Furthermore, these subdislocations can induce damage to the parietal cartilage, producing SLAP lesions. Posterior subluxation has also been reported in athletes requiring repetitive arm movements in front of the body, such as forward players in football and volleyball, softball, and baseball. In particular, throwing sports resulted in complaints of posterior shoulder pain during the follow-up period, was associated with posterior subluxation, and resulted in microscopic damage to the posterior parietal capsule complex.
Physical symptoms
Systematic evaluation includes observation of abnormal movement patterns and muscle atrophy, palpation to locate areas of pain, assessment of both active and passive range of motion, and measurement of muscle strength. rotator, neurovascular assessment, and finally tests for instability. Check the opposite shoulder for comparison
When assessing shoulder movement, carefully document any substitutions of thoracic scapula movement with brachial fascia, scapula swings, and other unusual patterns of motion. Atrophy of the perispinous muscles may indicate a rotator cuff tear or an upper shoulder nerve injury. Similarly, deltoid atrophy may indicate an axillary nerve injury.
Đánh giá bệnh nhân để tìm các lỏng lẻo của dây chằng nói chung, bao gồm khả năng duỗi khuỷu tay quá 10°, áp ngón tay cái vào cẳng tay, duỗi các khớp cổ tay trên 90° hoặc chạm lòng bàn tay của mỗi bàn tay xuống sàn trong khi giữ đầu gối duỗi. Mặc dù không có mối liên hệ trực tiếp nào giữa sự lỏng lẻo của dây chằng nói chung và sự mất ổn định của vai, nhưng có một số mối liên quan giữa sự quá dẻo và sự phát triển của bao khớp ổ chảo cánh tay.
A patient with an acute anterior dislocation, inability to self-align, holds the affected arm in a flexion and internal rotation. Before performing any manipulation, examine the neurovascular system carefully to rule out brachial plexus injury and, more specifically, axillary nerve injury. In older people (> 60 years old) or younger people who have suffered a major injury, be aware of the possibility of fracture related blow. Take a shot X-ray Testing is especially important before attempting to seal in such cases.
Pay careful attention to patients with undetected chronic (fixed) dislocations. Dislocations are usually posterior, although anterior, and often occur in patients with a poor history of alcohol use or dementia. In patients with fixed posterior subluxation, there is limited external rotation relative to the contralateral shoulder. Additionally, there is a flat palpation in the anterior part of the shoulder with a protrusion of the cranium and possibly some slightly raised and rounded spots posteriorly of the shoulder. The use of excessive force to attempt to seal such a patient carries the risk of neurovascular injury or fracture.
After careful neurovascular examination, it is important to assess active and passive range of motion. Differences between active and passive range of motion may suggest an associated rotator cuff tear or nerve injury.
It is especially important to identify subscapular tears in the case of shoulder instability, which is often overlooked. Patients with such lacerations have increased passive external rotation with the arm proximal to the torso, as well as a feeling of apprehension associated with this position.
Evaluation of muscle strength is also important. Significant external rotation weakness may indicate a rotator cuff tear. Similarly, weakness in internal rotation can result from a muscle tear under the shoulder. In this situation, the patient has an accompanying positive lift-off sign. If the patient is unable to rotate internally to perform this test, perform abdominal thrusts instead to determine the patient's ability to pull the forearm posteriorly toward the mid-abdomen while still holding the elbow. fold forward relative to this point. If the elbow is still behind the front of the mid-abdomen, there is a possibility of a tendon tear under the shoulder.
Various stimulation maneuvers and drawer tests have been described to assess brachial displacement and the direction of this movement. Neer and Foster originally described the fear test for frontal instability. When the patient is sitting or standing, place the symptomatic shoulder in a 90° position and maximally external rotation. Then, move the arm behind the plane of the shoulder blades and apply a force forward on the top of the arm. The patient withdraws his hand from the examiner or complains of an unsteady feeling in the shoulder expressing apprehension.
Complaints of pain are not specific to instability and may, in fact, be present with other conditions such as arthritis or rotator cuff disease. Kvitne and Jobe proposed a modification of this maneuver to increase its specificity for frontal instability. Place the patient in the supine position and perform the anxiety test as described above. Ask if the patient has a feeling of malaise or simply pain. Put back pressure on the arm, and ask if this force reduces feelings of fear or pain. This “re-entry procedure” increases the specificity of the diagnosis of instability if the patient reports decreased anxiety. If this move is simply pain relief, it is not unstable and may be associated with many other conditions, including SLAP lesions or conflict syndrome.
The inconsistency with the fear test led Gerber and Ganz to develop an anterior and posterior drawer test to assess whether the shoulder is moving too much from the side. Others have discovered the value of this testing method and have developed scales for shoulder laxity. This method is used during examination under anesthesia to confirm the extent and direction of shoulder instability.
Altchek, Hawkins et al proposed a classification scale for displacement of the brachial crest with the socket. Instability is rated on a scale of 0 to 3+ for all three directions. For the front and back drawer tests, a score of 0 represents no tip displacement, while movement of the tip upward but not over the bearing rim represents instability from 1+. The displacement of the tip over the rim of the socket with self-reflection is accompanied by a reduction in the force of rendering instability 2+. Frank dislocation and proximal locking beyond the socket rim are classified as unstable 3+.
A modification of the back drawer test allows the tester to elicit back anxiety. Perform this modification by placing the patient's arm in a 90° forward flexion and adduction while applying an axial force down the humerus. Pain and palpable slip and clack indicate injury and instability of the posterior parietal cartilage.
A modification of this test, known as the sulcus test, has been described for posterior instability. When the patient is sitting, use one hand to flex the shoulder in the direction of the socket and feel the back of the shoulder with the other hand. Then bring the closed arm in front of the shoulder blade plane; The tip of the arm may be dislocated. Then, bring the head behind the scapula plane; The tip can slide quickly into the socket. A palpable displacement and accompanying pain give a positive test.
The sulcus sign is essentially a lower drawer test. Unfortunately, a common misconception is that the large sulcus sign is asymptomatic, thus indicating inherent joint laxity, as a positive finding. The bottom line is that this maneuver must be related to pain and must reproduce the patient's symptoms to be clinically relevant as a finding of inferior instability. Perform this test with the patient sitting with their arms closed to their torso. Shoulder rotation is important in assessing shoulder instability. First, with the arm in a neutral rotation position, pull the crest downward, and estimate the distance between the apex and the crest. Graded on a scale of 0 to 3+: 1 cm distance is 1+, 2 cm is 2+ and 3 cm is 3+. Anatomically, a sulcus sign greater than 2+ indicates a capsule with specific capacity and laxity of the superior anterior capsule (rotational space). Externally rotate the arm and repeat the test. If the sulcus sign remains greater than 2+ with the arm lateral rotator cuff, then there is a marked deficiency of the superior capsule and there may be a large rotator cuff defect. This is the result of damage to the superior and medial alveolar ligaments, as well as the brachial cruciate ligaments. With this information before surgery, you will know that surgery to reconstruct this area with capsule displacement must be part of the surgery.
Four different types of multifocal lesions (MDIs) have been described:
- Type I: Total instability.
- Type II: Mainly anterior and inferior instability.
- Type III: Mainly posterior and lower instability
- Type IV: Anterior and posterior instability without inferior components.
Since the description of superior border cartilage by Andrews et al in 1985 and SLAP lesions by Snyder et al in 1990, several examination techniques have been developed to diagnose this disease. According to Andrews, the patient experienced increased pain with complete flexion and closure of the shoulder, accompanied by insertion and disengagement. Snyder states that the patient has pain when flexing the antagonist shoulder by extending the elbow and supine the forearm (biceps tension test).
Another useful diagnostic test is the compression-rotation test. When patient is supine, shoulder 90°, elbow flexed 90°. Apply compression to the arm to keep the meniscus from tearing (same as the McMurray test for the knee). O'Brien et al proposed a procedure that they believe is accurate for identifying upper border cartilage lesions. Place the patient's shoulder in a forward 90° flexion and then over the body. Ask the patient to flex the arm further to counteract resistance during internal and then external rotation. If pain occurs on internal rotation but no pain on external rotation, the test is positive. Unfortunately, this test does not differentiate between sacroiliac arthritis and a meniscus tear. However, this test is more useful than the other methods described above.
DIAGNOSE
Minimal radiographs are required to evaluate for acute dislocation or suspected subluxation in the anteroposterior (AP) and axillary positions. These images will allow to determine the exact position of the top of the arm relative to the socket. The Y scapula can also provide useful information about the position of the top of the forearm, but it is not as accurate as the armpit position. If a standard axillary position cannot be obtained, a Velpeau axillary position without removing the patient's arm from the sling will suffice.
The AP position of the shoulder with the arm internally rotated may show a Hill-Sachs lesion. The Stryker angle will also show a Hill-Sachs lesion.
The West Point axillary position may be helpful in a patient suspected of having an episode of instability. Image with the patient prone so that the anterior fossa is shown without overlapping apical shadows.
Adjunctive imaging techniques are useful when additional information about the three-dimensional structure and relationships of the joint is needed or to confirm the presence of a Bankart lesion. Computed tomography (CT) scans reveal trauma or bone abnormalities including alveolar hypoplasia, congenital anomalies, erosional abnormalities, and alveolar rim fractures. In addition, it allows to measure the size of the brachial cleft (Hill-Sachs lesion) in cases of chronic instability. When combined with intra-articular contrast, a joint CT scan also shows Bankart lesions and joint erosion.
Magnetic resonance imaging (MRI) with or without gadolinium is preferred, although unfortunately it is often used as a screening tool in the evaluation of patients. Instead, its role should be to confirm the presence of lesions that may require surgical management. It is accurate in detecting parietal cartilage pathology. Recent advances in MRI technology such as high-resolution rapid rotation and negative band imaging make it particularly useful for the detection of anterior and superior parietal cartilage lesions.
TREATMENT
Misdiagnosis leads to ineffective treatment. Patients or doctors can make these mistakes. A successful outcome begins with an accurate diagnosis followed by the specific treatment needed for that particular patient.
Conservative treatment
Studies of the natural history of traumatic shoulder instability have shown a high recurrence rate with nonsurgical treatment. Rowe and Sakellarides reported a recurrence rate of 58% in 398 patients with 53% follow-up. Subsequent studies have verified this trend. A large Scandinavian study found that the younger the age, the higher the recurrence rate, especially the trauma age under 20 years old. Hovelius et al reported a 10-year follow-up of 245 patients with 247 primary dislocations. Recurrent dislocation requiring surgery occurred in 34% among 99 shoulders aged 12-22 years, 28% among 57 shoulders aged 23-29 and 9% among 91 shoulders aged 30-40 years.
Although Watson-Jones' original claim in 1948 that motionless completely within 4 weeks produces complete stability, others have not reported such successful results. In fact, the success of fixation can vary. Rowe and Sakellarides reported that immobilization for 3 weeks reduced the recurrence rate. Henry and Genung reported no significant improvement with immobilization. Aronen and Regan found that the recurrence rate was reduced to 25% if the first dislocation was treated with isometric, isotonic, and isokinetic exercises. Burkhead and Rockwood assigned a shoulder therapy exercise program to traumatic or non-traumatic patients. In the post-traumatic subluxation group, 16% showed a good response to the program Rehabilitation, while the 87% non-traumatic subluxation group without psychological problems had good to excellent results. Hovelius et al reported that the type of dislocation and the duration of initial treatment did not affect the recurrence rate.
As such, it is clear that the most important factors for determining recurrence of post-traumatic instability are age and activity level.
Surgical treatment
Surgery is often recommended if instability recurs despite good physical therapy and activity modification. The goal of surgery is to restore stability to the shoulder with minimal loss of range of motion. All shoulder tricks designed to stabilize the shoulder involve a loss of motion. Current surgery for anterior shoulder instability attempts to restore normal anatomy without unduly straining the ligament. In certain cases, such as in young people at higher risk of re-dislocation and athletes who plan to continue participating in sports that put their shoulder at risk, surgery can be performed after the first dislocation. For traumatic anterior or posterior instability, surgeons can confidently inform their patients that their chances of returning to near-normal function are greater than 90%.
The procedures described for the management of anterior instability can be grouped into anatomical and non-anatomical. Anatomical restorative sutures include reattachment of the capsular cartilage structures to the socket as well as the re-establishment of appropriate tension in the capsule and ligaments. Bankart, Thomas, and Matsen suggested that only sutures were needed to restore the marginal cartilage and its attachment capsule without shortening the anterior ligamentous and capsule structures. Shortening of the capsule and the subscapular muscle can be used in the absence of a meniscus tear, suggesting that a dilated capsule is the cause of the instability. Others describe internal reduction of the capsule or subscapular attachment as part of a Bankart restoration. Wirth et al. explain that the reduction of joint capsule volume is as important as the repair of Bankart. Subcapsular shortening was performed similarly to the original description by Neer and Foster. Anterior capsule shortening is designed to reduce circumferential capsule volume. This is accomplished by making an incision in the capsule and sliding the flaps over each other to stiffen and reduce the volume of surrounding capsule tissue.
Non-surgical surgical procedures are designed to limit external rotation and provide anterior support to prevent dislocation. They include tricks Putti-Platt, which involves shortening and folding of the muscle below the shoulder; the Magnuson-Stack procedure, which is to attach the muscle below the shoulder; the Eden-Hybbinette procedure, which grafts the iliac crest bone in front of the socket; and the Bristow-Latarjet procedure, which is a transfer of the cranium with an anteriorly attached connective tissue below the socket through or around the subscapular muscle. The disadvantages of the open technique include damage to the muscles below the shoulder, loss of external rotation, and difficulty gaining strength and returning to sports.
The advent of arthroscopy has brought new curiosities and challenges to the management of anterior instability of the shoulder joint. Endoscopy showed better overall function. The arthroscopic approach has several advantages over the open approach. It gives a better image of intra-articular pathology, limits dissection to prevent tearing and restores subscapular muscle, reduces scarring and loss of strength after surgery, reduces recovery time, and reduces loss of range of motion. movement, pain relief, and postoperative bleeding. Alternatively, the test can be done in an outpatient setting.
Arthroscopic rehabilitation in high-demand patients (younger patients, military personnel, athletes, and high throwers) has been shown to be effective in the recent literature. However, in a study comparing open surgery with arthroscopy in athletes, open surgery resulted in a lower failure rate.
Endoscopic failure was associated with persistent or recurrent Bankart's lesion, large Hill-Sachs lesion, alveolar bone loss, number of dislocations, number of revision surgeries, concomitant joint laxity, and duration. immobilization after surgery. Bone loss of more than 25% anterior to the subfoveal socket, whether progressive or acquired, is generally considered a contraindication for arthroscopic repair.
BACKGROUND AFTER SURGICAL
Phase I: from 0-4 weeks after surgery
- Purpose:
+ Repair firmware protection.
+ Reduce inflammation, reduce edema.
Allows early movement to avoid muscle atrophy.
– Attention: Wear shoulder brace for 4 weeks, wear continuously day and night.
+ Do not actively exercise and stretch the shoulder joint.
+ Do not actively exercise biceps brachial muscles.
+ No running.
+ Do not strain the arm muscles within 6 weeks.
– Rehabilitation treatment in the first 0 – 2 weeks after surgery:
+ Apply cold shoulder joint for 10 minutes every 3 hours to reduce swelling and pain.
+ Wearing a brace, not moving the shoulder joint: moving the wrist and hand in the brace.
+ Wear a brace with elbow joint close, allowing active pronation and elbow movement several times a day.
- Rehabilitation from 3 to 4 weeks after surgery:
+ Continue to apply cold compresses to the shoulder joint
+ Passive exercise of shoulder joint: allows passive horizontal shoulder, shoulder close 80°
+ External rotation (passive rotation) intermediate position, gradually progressing to external rotation 30°
+ Practice active muscle contraction in the brace several times a day, practice walking
+ Can operate fingers like using Computer if the activity does not cause shoulder pain.
Phase II: from 5-7 weeks after surgery
- Purpose:
+ Gradually increase shoulder joint range of motion
+ Exercise muscle strength, reduce inflammation, reduce edema
+ Strengthen shoulder joint activity.
- Attention:
Avoid excessive external rotation of the shoulder joint.
+ Active movement only when the patient can rhythmically operate the shoulder and arm.
+ No biceps resistance training for 6 weeks
+ Do not lift heavy objects, avoid movements over the head.
- Movement exercises:
+ Exercises gradually increase from passive movement to active movement with assistance and active movement of the shoulder joint
+ Do shoulder flexion exercises at the patient's tolerance level
+ Shoulder closure at a tolerable level
+ Practice 50° external rotation, 60° internal rotation, from 90° elbow flexion position.
Phase III: from 8-12 weeks after surgery
- Purpose:
+ Protect the incision
Regain full range of shoulder joint range of motion
+ Gradual increase in muscle strength
+ Increases the role of muscle control
Increases the role of neuromuscular control.
- Attention: control internal and external rotation of the shoulder joint, continue to protect the biceps.
Strengthen the biceps
- Exercises: Exercise to regain full range of motion of the shoulder joint.
+ 180° gấp folding movement
+ Rotate the shoulder joint 90° from the closed shoulder position
+ Strengthen shoulder belt muscles.
+ Wall crawling exercise
+ Rotate in the shoulder behind the back
Intra-shoulder rotation from 90° . shoulder flexion
+ Practice daily activities
+ Up to 9 weeks: start putting your hands behind your head to strengthen your internal and external rotator muscles
Up to 11 weeks: range of motion exercises
+ Rhythm practice
+ Practice daily activities
+ Practice hand and shoulder activities.
Stage IV: from 12-16 weeks after surgery
- Purpose:
+ Regain full range of motion of the joint
+ Neuromuscular control
+ Control hand function, use hands in daily activities.
EXERCISES: CONTINUE MAINTAINING THE EXERCISES STAGE III
+ Maintain active and passive range of motion of the shoulder joint
Avoid returning to daily activities and sports activities that cause shoulder pain
DRAW phase: from 16-24 weeks after surgery
- Prepare to return to sports and physical activity
- Continue strengthening exercises
- Be careful when carrying heavy objects
Complications AFTER SURGERY TREATMENT
Instrumental complications
The simplest method to prevent complications from the device is to not use it at all. Instrument failure or loosening may occur weeks or years after surgery.
Bioreactivity for Implants: Absorbent devices are less reactive than metallic materials. However, absorbable devices can be eroded by biological reactions. If this response is excessive, clinical effects may occur. Although significant mixed reaction with anchor polyglyconate and polylactic acid is infrequent, it is clearly possible and visible with other biological materials, the extent of which depends on the specific material.
Infection
Infection is a very rare complication following shoulder instability surgery.
Painful
Pain usually improves after shoulder destabilization surgery.
Complications of open surgery
Subscapular muscle tears following anterior instability repair are increasingly recognized as a cause of postoperative failure and injury.
Osteoarthritis và xung đột dưới mỏm quạ sau đục xương ổ chảo sau cũng được ghi nhận, đòi hỏi phải phẫu thuật thay khớp vai.
Complications after endoscopy
Recurrent instability, caseation Arthralgia, cartilage loss, axillary nerve damage were also recorded but accounted for a very low rate.
Complications of conservative treatment
Failure of nonsurgical management may be manifested by recurrent symptoms of instability (dislocation, subdislocation, or pain) despite adequate monitoring management and appropriate activity modification.



