Table of contents
OUTLINE
Brief history of amputation surgery
Cutting surgery amputee dates back to very early in medical history, were barbaric punishments in ancient societies, the stopping of bleeding by tying the cutting tip or dipping it in boiling oil. In the early sixteenth century, Ambroise Paré (France) described more closely the function of the amputation and was the first to tie up the blood vessels during amputation and proposed a prosthetic limb. In the seventeenth century, Morel introduced how to bandage the stump,... Until recently, after the work of Rolf-Diderich, this surgery has been studied extensively. Amputation is no longer a mere surgery but has become a specialty with separate principles of treatment, monitoring and evaluation, in which there is always a combination of: orthopedic trauma, Rehabilitation and psychotherapy.
The purpose of amputation is not only to amputate the limb but to restore the function of that limb. After World War II, amputation saw many advances in technology, as tens of thousands of young soldiers were amputated as a result of the war. Advances in many fields have made amputation a major specialty: muscle and bone reconstruction techniques, understanding of biomechanical principles in body movement, human bone, innovative discoveries. new types of prostheses along with a measurement of the patient's capacity to consume while using the prosthesis.
In 1963, at the 6th Prosthetics Conference in Copenhagen, Weliss (Balan) suggested the use of prostheses after amputation without waiting for the wound to heal. These advances have led to the exciting results of reducing the number of repeat surgeries to correct the stumps, allowing amputees to lead a near-normal life in a short time. Many authors define amputation as a procedure aimed at removing part or all of a limb. If the incision goes through the bone, it is called a true amputation; if the cut goes through the joint space, it is called an amputation.
Pathophysiology of the stump
After amputation, the amputated tissues have the following changes:
Local changes
- Bone
- Osteoporosis at the tip of the coccyx spreads upward, sometimes spreading to the joints. Osteoporosis appears clearly on the 10th day and lasts after a long or short time depending on the patient's general condition, sometimes up to years.
- The ends of the bones are shrinking. Particularly in children, long bones are faster than muscles and skin, especially at the cutting site near the synovial cartilage. Therefore, the stump in children is often small, pointed and the bone tip protrudes out of the skin, so it is not possible to make a permanent prosthesis immediately, but must wait until adulthood and repair the stump before installing a prosthesis.
2. Muscle skin and other software
- Skin: uneven shrinkage depending on location. In general, the skin is thin, with less subcutaneous tissue, not attached to deep tissues, and more shrinkage.
- Muscles: The muscles in the superficial area have roots, which are attached to each other, and contract more than the deeper muscles. Contraction occurs immediately after cutting and increases further.
3. Blood vessels
-
Động mạch và tĩnh mạch đều teo nhanh, sau 2 tháng cắt cụt thì động mạch đùi nhỏ lại chỉ bằng động mạch quay, động mạch cánh tay nhỏ lại bằng động mạch bên ngón tay.
4. Nerves do not atrophy like other soft tissues, but tend to elongate, but mainly the axons of the nerve This elongation is caused by the resistance of the stump causing them to curl. form a tumor called a neuroma. In gliomas with sensory and motor branches, the sensory branches still conduct stimuli centrally. Therefore, after amputation, the patient still has the feeling that the limb still exists as if it has not been amputated, which is the phenomenon of "ghost limb" after amputation. The physiological phenomenon of "chi ghost" will gradually decrease and completely disappear after a period of adaptation. Neuromas can cause reflexes such as arrhythmias, heart attacks, hypertensive attacks, or asthma attacks.
Body transformations
Amputation greatly affects the activities and health of the patient. People with upper limb amputation are less likely to experience reduced activity, so there are few major changes. In contrast, people with lower limb amputation often have more reduced activity, so they are more prone to obesity.
Indications for amputation in trauma, wounds
Today, the indications for amputation are narrowed thanks to advances in science in general and medicine in particular, such as resuscitation, antibiotics, grafting techniques, and transportation. Therefore, only amputation is done when there are no conservation conditions or no more conservation measures.
Indications for first-term amputation
- Wounds come soon
- Natural amputations: the limb is completely severed or partially attached to the skin and tendon, which is not available for anastomosis.
2. Injuries come late
- When the tourniquet has been booked for a long time but held under the place where the garage is damaged caseation Due to lack of nutrition, amputation is required to save the patient's life.
- Wounds with anaerobic or other severe infections for which conservative treatment has not been successful.
Indications for late amputation
- Injury to many blood vessels but hopefully can still be preserved, leave it for a while, if you see that the undernutrition of the limbs is getting worse, then amputation should be indicated.
- The infected limb can still be treated conservatively, but after a period of treatment, the infection becomes more and more serious, threatening the patient's life. Amputation at this time aims to remove the infection site most thoroughly to save the patient's life.
Indications for second-term amputation
- Cases that have undergone plastic surgery, but cannot return proper limb function because of crooked and contorted postures, sometimes more entangled in work and daily life, need amputation to replace with prosthetic is more appropriate.
- Cases inflammation of the bone, arthritis destroyed much, tends to spread, but the ability to treat conservatively is no longer available.
- Cases that have been amputated or removed, but now the old apex is bad or unsatisfactory for fitting a prosthetic limb (the coccyx has osteomyelitis, subcutaneous osteophytes, ulcers, etc.) or is painful, burn neuropathy pain).
Indication of amputation in war
During war, the amputation designation is essentially the same as peacetime. However, it also depends on equipment, technical level, ability to receive treatment of each line in front of a large number of wounded soldiers, so the indications for amputation are often more extensive than in peacetime. But also need to be careful to ensure two requirements:
- Save the lives of wounded soldiers, save as much of the patient's limbs as possible
- Leave the wound open.
Amputation technique
Amputation methods
Round cutting method
- Flat circular cutting is a classic cutting method, cutting the soft and bone at the same level, the blade is placed perpendicular to the limb axis. This method is quick and simple, the tip of the stump is fully exposed from the bone to After the round cut, the stump will lack skin and muscle, so the bone will be protruding out, so it is necessary to treat the two new stumps. leather and prosthetic limbs. Therefore, only apply flat round cut to the case of gangrene that produces gas or tourniquet for too long but the lower part of the tourniquet has been necrotic or in case the patient is not strong enough, emergency surgery is required to save his life. patient's life (Figure 18.1).
- Round funnel cutting is a method that calculates skin and muscle contraction according to the position of bone sawing, so it is also called a typical amputation method (Figure 18.2).
Specifically:
- Identify bone saw landmarks
- Cut the skin below the ostomy mark one diameter anteroposterior of the ostomy site
- Cut muscle layer by layer
- Superficial muscle cutting according to skin contraction level
- Cut the deep layer muscle at the level of the superficial muscle contraction or at the level of the bone saw.
![Outline of Amputation Surgery 2 Cắt Tròn Hình Phễu [2]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Cat-tron-hinh-pheu-2-211x300.png)
+ Cut the bone at the intended position after lifting the muscle above the level of bone sawing.
In the slender limbs, if it is difficult to lift the skin and soft part up to see the bone, one or two more lateral lines can be torn, the top of the notch must be higher than the level of the bone saw.
- Open circular cutting (Pi-rog) does not specify anterior bone cutting level, bone cutting level depends on software cutting level.
+ Cut the skin: cut the skin in the healing place right above the injured area, whichever side the skin shrinks a lot, the lower side will be cut.
+ Muscle cutting:
- Superficial muscle cutting according to skin contraction level
- Deep layer muscle cutting according to the level of superficial muscle contraction
+ Cut bone at the position where the deep muscle layer has contracted.
As with typical circular resection, open circular resection may be accompanied by a lateral slit to release compression as the edema spreads upward.
Open circular cutting is indicated when:
- Broken limbs, wounded soldiers stunned severe, amputated to cure the cause of the shock.
- Extremities of widespread infection, anaerobic infection. Oval cutting method
Pear-shaped cut, soft enough to wrap the stump after removing knuckles, shoulder.
Flap cutting method
![General Amputation Surgery 4 Cắt Hai Vạt Bằng Nhau Và Cắt Hai Vạt Không Bằng Nhau [3]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Cat-hai-vat-bang-nhau-va-cat-hai-vat-khong-bang-nhau-3-300x189.png)
![Outline of Amputation Surgery 5 Kỹ Thuật Băng Mỏm Cụt Trên Gối [3]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Ky-thuat-bang-mom-cut-tren-goi-3-300x200.jpg)
![Outline of Amputation Surgery 6 Kỹ Thuật Băng Mỏm Dưới [3]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Ky-thuat-bang-mom-duoi-3-300x246.jpg)
![Outline of Amputation Surgery 7 Kỹ Thuật Băng Mỏm Cụt ở Tay [3]](https://bsvothanhtoan.com/wp-content/uploads/2023/04/Ky-thuat-bang-mom-cut-o-tay-3-300x144.jpg)
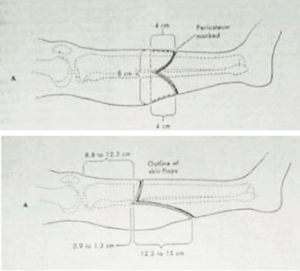
The two flaps are equal, short and long depending on the location and characteristics of the wound.
The crest between the two flaps is always higher than the bone saw and above the masonry (if any). The slit must cover all layers of skin, tendons and muscles.
Nguyên tắc tính chiều dài của skin flap: tổng độ dài hai vạt bằng hai lần đường kính trước sau chỗ định cưa xương.
- Equal flap is usually applied in the limb where the muscles are symmetrical on both sides of the limb (1/3 mid thigh, 1/3 middle forearm), the scar will be in the middle of the stump.
- Cut two unequal flaps when the muscle groups are in disproportionate position, such as the middle third of the leg, or in a war wound, in order to take advantage of good soft tissues.
In practice, to quickly and cut the muscle surface flat, the tip of the amputation knife can be placed at an angle between the two flaps, from there, through the knife to the other corner of the two flaps, the blade is right in front of the bone, at 45 degrees. relative to the bone axis. Pull the knife down in the oblique mode, we have created the front flap, the back flap also does the same.
Then proceed as a general rule. If the amputation is caused by a war wound, it is not sutured, but only needs to put the two flaps together, put large gauze and bandages, doing so, the bones and blood vessels have been covered (this method is called flap amputation. left open).
Amputation tools
- Long knife (amputation knife): how long the knife is depends on where the amputation is intended
- Saw: usually use table saw or frame saw
- Bone retainer
- Remove periosteum, file bone
- Pliers to chew bones, pliers to cut bones
- Tools to protect software when sawing bones: discs, big and long antlers
- Thin sharp blade for cutting nerves (usually using a razor blade)
- Lidocaine 1% for pre-excision nerve block.
Value of amputation position at each limb segment
Upper limb
- Fingers and hands:
+ Thumb: must be preserved because its value is equal to that of other fingers. The thumb compared with other fingers is a necessary movement in daily life and work.
+ Index finger:
- If the whole finger is lost then:
- Should keep hand bone 2 for workers equal to
- Should remove both hand bones 2 for technicians who need to be skillful. Removal of the second metatarsal so that later the middle finger can be used instead of the index finger.
Middle and index fingers:
If both of these fingers are removed, the 3rd and 4th metatarsal bones should also be removed so that the fingers can be closer.
Pinky and ring fingers:
If both of these fingers are removed, the bones of the hand should be kept intact and strong.
- Forearm: the best position is the lower 1/3, the remaining segment is about 15 - 17 cm from the elbow (at least 9 cm)
- Arm: the best position is the lower third, the rest is about 13-22 cm, from the apex of the shoulder
- Shoulder joint: since prosthetics cannot be worn, try to leave a portion of the head above the humerus, even if it is less, it is better than removing the joint.
Lower extremities
- Toe:
Amputation of the thumb or the other four fingers is a reluctant case because it makes it difficult to walk quickly and run.
- Foot:
It is best to cut across the metatarsal bone at the base of the bone. Today, Chopart or Lisfranc dissection is rarely used.
- Ankle:
+ Pirogop technique: creating a good stump without pain, walking easily, ensuring the relative length compared to the healthy leg.
+ Syme-Ollier technique: also creates a good stump but lacks the length compared to the healthy leg.
- Legs: it is best to cut the lower third of the leg, the remaining part is about 10-15 cm from the tibial plateau
- Thigh: the lower third is best amputated, the remaining segment is about 25-30 cm from the great trochanter
- Knee joint: do not remove the knee joint. If necessary, Gritti surgery should be performed
- Hip joint: do not remove the hip joint, try to keep part of the head above the bone
femoral.
Technical requirements
A properly performed amputation must meet the following requirements:
– Good stump
+ Soft scars, do not stick to deep organizations
+ No pain
+ Skin is not ulcerated
– The remaining limb must be able to carry a prosthetic limb
+ Long enough
+ Muscles do not atrophy, move well
The upper joints must move normally
General principles of engineering
- Insensitivity
Depending on the amputation site and the patient's general condition, an appropriate method of anesthesia is selected such as: anesthesia, intraosseous anesthesia, spinal anesthesia or local anesthesia combined with regional anesthesia.
- Temporary hemostasis with garo after the Esmarck tape has been rolled
- Cut the skin flap.
+ Skin and shallow scales are cut at the same time.
+ Before cutting, use methylene blue to draw a cut line on the skin.
- Muscle cutting: there are two ways to cut
+ Cut immediately to the bone (war wound, gangrene wound, ...)
+ Cut each layer:
- Major vascular treatment
+ The blood vessel must be tied to the cutting level of the muscle it nourishes.
Large blood vessels need to be tied twice.
+ Small blood vessels only need to be tied once.
- Nerve
+ Must cut higher than the bone saw.
+ Cut the nerve to use a sharp knife, cut a neat and definitive cut (usually using a razor).
+ For the sitting nerve, it is necessary to block the lidocaine before dissection (see the article Fem amputation).
+ Do not inject alcohol or other stimulants into the nerve endings after cutting.
- Bone Saw
Before sawing the bone, use a disc or gauze to lift the surrounding muscles up, cut the periosteum where the bone is to be sawed and cut from the top down. The purpose of periosteal resection is to avoid tearing the periosteum in the saw area, and to avoid the occurrence of thorns around the saw site. For a limb with two bones, the movable bone is cut first, the fixed bone is cut later, but when sawing, it must start at the fixed bone first. After sawing, the ends of the bones must be smoothed and then washed off the bone humus with warm isotonic saline.
- Slowly loosen the garo and stop additional bleeding, correcting the stump.
+ Note: Before loosening the garo, it is necessary to inject heart support with caffeine coramin.
- Stitch the stump (within allowable conditions).
+ Sew symmetrical muscle groups together with Catgut thread.
+ Sewing scales and skin with linen thread.
+ Place drainage in the first 24-28 hours.
- After surgery, use high-dose systemic antibiotics
Monitor for bleeding and infection.
COMPLAINTS AND PARTNERSHIP CARE
Complications after surgery
- Hematoma of the stump
- Infection
- Caseation
- Poor posture shrinkage
- Nerve tumor
- U are sensitive to ghosts.

Post-operative care
- The stump is bandaged: the stump is bandaged with an elastic bandage with diagonal bands, slight pressure from the tip of the stump to the base of the limb. Avoid circling the bandage The goal is to prevent edema and shape the stump during the period starting from the surgery to the time of wearing the prosthesis.
After 48-72 hours, remove the drain, 2 weeks after the incision is removed. In patients with vascular disease, sutures should be removed after 2 weeks, not early because the skin of the stump is not nourished enough in the first days, it is easy to open the incision.
- Postures to avoid: these are the positions that interfere with the later operation of the stump. Common positions are ankle extension, knee flexion, groin flexion, elbow flexion, arm closure, these are the patient's pain relief postures. It is necessary to put the opposite position.
- Exercise the stump: start soon after surgery and continue until able to use prosthetic limb competently in order to prevent: bad posture of the stump, creating a good stump of good length correct, slim head shape, scar is not shrinking, not sticking and creating a balance between muscles.



