Table of contents [hide]
1. DEFINITIONS
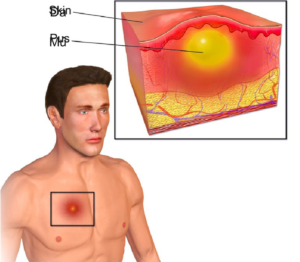
Abscesses, boils, and boils in the extremities are acute pus-filled sores that form in the soft part of the extremities accompanied by common symptoms of swelling - heat - redness - pain.
2. Epidemiology
- Abscess rates increased throughout the 1990s; related to the increase Staphylococcus aureus methicillin-resistant (MRSA)
- Since the 2000s, the incidence of abscesses has been stable
- Abscesses can develop anywhere, but are most commonly found on the trunk, extremities, armpits, and buttocks.
3. CAUSE
3.1 Pathogens
- – aureus (75% cases):
+ S. aureus sensitive to methicillin (MSSA)
+ MRSA
- Multi-bacteria:
+ S. aureus (golden staphylococcus)
+ Streptococcus pyogenes (group A streptococcus)
+ Gram-negative bacilli
+ Anaerobic bacteria – Rare agent:
+ Mycobacteria
+ Nocardia
Fungi (cryptococcus, blastomycosis).
- Not due to microbiological agents: caused by infusion of the drug is irritated.
3.2 Risk factors
- Loss of skin integrity due to:
Trauma (eg, scratches)
+ Inflammation (eg, atopic dermatitis) + Intravenous administration.
- Ức chế miễn dịch (ví dụ, đái tháo đường)
- Pre-existing skin infections (eg, folliculitis)
- Fat
- Location MRSA – Varicose veins
- Lymphedema.
4. Pathophysiology and pathology
- Breaks down the skin barrier → introduces infections/pathogens
- Local cell damage and necrosis causes release of cytokines
- Inflammatory cells are attracted to the site of infection/irritation, to encircle and destroy the pyogenic bacteria
- Creation of a fibrous barrier at the circumference:
+ Prevent the spread of infection
However, it also inhibits the infiltration of immune cells and antibiotics.
- Infections in enclosed spaces (eg, blocked sweat glands or perianal glands, hair follicles) also facilitate the development of an abscess.
- The low pH inside the abscess cavity further reduces the effectiveness of antibiotics – Pathology: the structure consists of two components:
+ The septum: the inner layer is a fibrin network, the middle is a young connective tissue, the outside is a fibrous organization + The cyst contains: contains pus, the properties depend on the type of bacteria:
- Sticky pus, milky cream color, odorless: staphylococcal abscess
- Diluted pus, pus-serum phase: streptococcal abscess
- Dirty gray pus, rotten smell: caused by anaerobic bacteria.
5. CLINICAL
Abscesses progress through two stages.
5.1 Diffuse inflammatory phase (onset period)
- The patient comes to the clinic because of pain, continuously increasing, localized in one area of the body (soft parts). Signs of systemic infection: fever, chills, lethargy, headache.
- Examination of an array reveals four basic symptoms:
+ Hard in the center and caked on the outside
+ Hot
+ Red
Pain when touching.

– Attached can detect:
+ An inlet: is a small wound, an injection site under the skin or muscle
Diffuse signs: red line of lymphadenitis, acute lymphadenitis
A pre-existing medical condition that is the most common aggravating factor is diabetes.
5.2 Stage of pus accumulation (after 5 ─ 7 days)
- The sharp pain disappears and the pain increases with the feeling of a pulse, causing the patient to lose sleep
- More severe systemic signs: persistent or fluctuating high fever, more fatigue, polymorphonuclear leukocytosis on blood test
- Mảng cứng khu trú lại, giới hạn rõ dần, có dạng một khối u đóng bánh ở viền ngoài, bây giờ sờ thấy dấu chuyển sóng (fluctuation): hai đầu ngón tay đặt cách nhau vài centimet ở hai cực của ổ mủ, khi đẩy. Dấu hiệu này có ở mọi hướng của ổ áp-xe. Khác với cơ vùng đùi dấu hiệu này chỉ có khi tìm theo chiều ngang của thớ cơ thẳng đùi.
5.3 How hot abscesses progress
- If the abscess is discovered and incision is made to drain the pus, take the pus cultured bacteria to make an antibiotic chart and use the scar within 5-7 days.
- If left untreated, a hot abscess can break into the skin on its own and leak pus. Purulent stasis can cause complications:
+ Local and regional: acute lymphadenitis, lymphadenitis, purulent lymphadenitis
+ Body as a whole: bacteremia, septicemia
+ Abscess turns into diffuse inflammation if the patient has an additional chronic disease such as diabetes, hot abscess can aggravate existing disease, for example diabetes.
6. PROCOLICIOUS
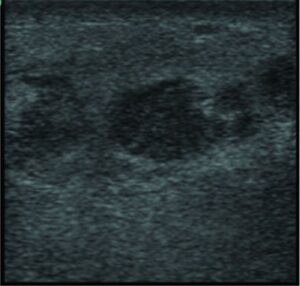
6.1 Diagnostic Imaging
- Ultrasound confirmed hypoechoic mass due to fluid retention; may be accompanied by foreign body
- X-ray: soft tissue swelling, helping to detect signs of cancer, fractures when abscesses are infected with tumors, fractures
- Contrast tomography is used in some cases of more extensive cellulitis or necrotizing fasciitis or abscess to show ring-enhanced lesions.
6.2 Tests
Unnecessary under normal circumstances – Blood collection and wound culture if:
Severe systemic manifestations
Presence of widespread cellulitis
+ Elderly patient
+ Recurrent infections
+ Does not respond to initial antibiotic
Immunodeficiency (eg, neutropenia, diabetes mellitus)
Special circumstances (animal bites, unusual exposures)
- Complete blood count: usually polymorphonuclear leukocytosis
- VS, CRP: usually increase
- Microbiology: culture specimens usually give positive results; Common are bacteria living in the skin such as yellow/white staphylococcus, streptococcus. In addition, Eberth bacilli, pneumococcal, gonococcal, anaerobic bacteria can also be seen
- TB PCR: if TB-associated abscess is suspected
- GPB: if superinfected abscess of tumor or tuberculosis is suspected.
7. CLASSIFICATION
- Simple software infection: skin, muscle
- Related to bone infections: from osteomyelitis, the prognosis and treatment are more complicated.
8. DIAGNOSTIC DIAGNOSIS
- Cellulitis: a common bacterial skin infection that affects the deeper layers of the dermis and subcutaneous tissue. Presents as an erythematous, edematous area that feels warm and tender to the touch. The most common is due to aureus and S. pyogenes cause. Diagnosis is usually clinical and antibiotic management is based on the suspected causative agent.
- Necrotizing fasciitis: a rapidly progressing infection resulting in extensive necrosis of subcutaneous tissue, fascia, and muscle. Most commonly due to Streptococcus group A causes but often involves other bacteria in a mixed infection. Manifestations of necrosis, blistering, rash and purple skin discoloration. Management is urgent surgical treatment along with broad-spectrum antibiotics.
- Dermatitis: a general term for an edematous skin rash. Caused by an infection or allergic reaction, usually not by bacteria. The diagnosis is established clinically. Treat with topical antihistamines and steroids.
- Folliculitis: localized inflammation of hair follicles or sebaceous glands primarily due to aureus cause. Manifested as erythema, papules, pustules and painful inflammation. Clinically diagnosed and treated with skin-clearing antibiotics and sometimes systemic antibiotics.
- Impetigo: a highly contagious skin infection of the upper epidermis. Do aureus or Streptococcus caused by group A. Appears an erythematous area covered with small blisters, pustules, and/or honey-colored crusts. Treat with antibiotics.
- Staphylococcal burn syndrome: a blistering skin disorder caused by a local infection usually caused by aureus. Presented with fever and widespread, tender erythema, intradermal vesicles and superficial skin shedding, leaving a red, “scaly” appearance. Treat with intravenous antibiotics.
- Epidermoid cyst (sebaceous cyst): Skin cysts are the most common, usually presenting as skin-colored nodules, sometimes with a dot in the middle. Clinically diagnosed and treated with surgical resection or follow-up. It is possible to become infected a second time and turn into an abscess, in which case the cysts present as tender, erythematous, mobile nodules that often drain spontaneously.
- Hidradenitis suppurativa (inflammation of the purulent sweat glands): Chronic suppurative infection of the sweat glands manifests mainly in the interstitial regions (armpits, groin, under the breast folds). Hidradenitis suppurativa usually presents as a nodule on the skin and induration is often associated with anastomosis of the sinuses. The diagnosis is confirmed clinically and treated with antibiotics and surgical resection.
9. TREATMENT
9.1 Outpatients
9.1.1. Indications and methods of treatment
- Surgery: performing minor surgery to drain pus is the main treatment for abscesses larger than 5 cm in size. For abscesses of 2–5 cm or multiple abscesses, or for patients with systemic symptoms, cardiovascular risk factors should be considered for medical treatment.
- Medical: use antibiotics appropriate to the causative agent. Use of oral antibiotics for 1 to 4 weeks depends on individual patient response. If the abscess is caused by tuberculosis bacteria: take anti-tuberculosis drugs for 12 months.
- Take care of the wound under the control of medical personnel.
9.1.2. Monitor
Educate patients on signs of treatment and when to monitor at home.
- Signs of response to treatment
+ Local: reduce swelling, heat, redness, pain, exudate
+ Whole body: healthy, able to eat and sleep, no fever - Follow-up period at home: 2 weeks.
9.1.3. Re-examination
- Time of follow-up: after 1-2 weeks of follow-up or as soon as there are abnormal symptoms, acute symptoms do not tend to recede due to unresponsiveness to treatment.
- Conduct: necessary laboratory tests, prescribe appropriate and specific drugs in each follow-up visit.
9.2. Boarding
9.2.1. Indications and methods of treatment
- Indications: large abscess with widespread cellulitis around; severe signs: skin necrosis, sepsis, the elderly with many underlying diseases, young children, patients who have been treated with oral antibiotics but have not been effective
- Conservation: antibiotics, pain relief
- Surgery: incision to drain the pus, drainage is still the preferred choice. Anesthesia can be used for large abscesses. Consider drilling into the bone to drain the bone.
- Wound care.
9.2.2. Drugs used
- Antibiotics are given intravenously for 1-2 weeks depending on response to treatment. Then switch to oral antibiotics for 1 to 4 weeks.
- If the abscess is caused by tuberculosis bacteria: take anti-tuberculosis drugs for 12 months.
Note: specify the content, time of use, contraindications, warning of poisoning and drug interactions.
9.2.3. Monitor
Signs and duration of follow-up in hospital.
Signs to watch for
- Signs of response to treatment
+ Local: reduce swelling, heat, redness, pain, exudate
+ Whole body: healthy, eating, sleeping, no fever - Follow-up time in hospital: 1 week.
9.2.4. Re-examination
- Time for re-examination: 1-2 weeks after discharge
- Conduct necessary laboratory tests, prescribe appropriate and specific drugs in each follow-up visit.
List of drugs used:
Drugs: use broad-spectrum antibiotics initially. Suggested: amoxicillin + clavulanic acid (augmentin) 1-2 g 3 times a day, 1 vial slow intravenous (TMC) or cefuroxime 750 mg, 2 vials 3 times/day. Combination: gentamicin 80 mg, 2 times a day, 1 vial of TMC.
Duration of use: 4 days, until the antibiotic chart is available.
10. COMPLEX
Sepsis, necrosis, osteomyelitis.





