Table of contents [hide]
OUTLINE
Burns are injuries to the body, dating back to when the human race was formed and developed.
Burns can be shallow or deep, causing damage to the skin, changing the structure of the skin, the composition of the skin, and the subcutaneous tissue. Sometimes causing systemic disturbances.
According to the development of mankind and society, today we also know more burns caused by chemicals, radiation, and electricity.
Most burns are caused by accidents in daily life activities (cooking, ...).
REASON
Due to dry or wet heat, the temperature causes burns to damage cells > 45oC
Due to the electric current causing deep local damage, electric shock, cardiac arrest, and respiratory arrest may occur. Because radiation depends on the type of ray, the intensity.
Due to chemicals depending on the chemical, concentration, contact area.
Clinical and Paraclinical ASSESSMENT
clinical
Burn area
RULE NUMBER 9:
- Head - face - neck 9%, chest 9%
- Belly 9%
- Full back 18%
- Hand 9%
- Pin 18%
- Genitals 1%.
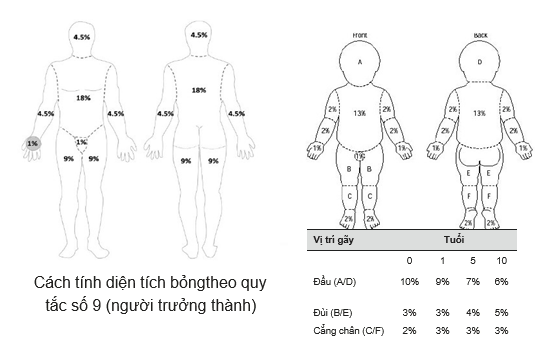
Method 1.3.6.9.18 of Le The Trung, National Institute of Burns.
Palm method: using the patient's hand size to estimate the burn area, about 1%, usually applied to small burn areas.
By depth (National Institute of Burns):
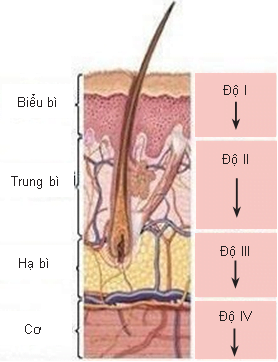
- Grade I: Superficial dermatitis, dry red skin, only the epidermis is affected, little burning pain, average healing time is about 1 week.
- Second degree: Burns of the dermis, with caseation Epidermis (with germ cell layer, basement membrane intact), with vesicles, usually heals within 1 to 2 weeks.
- Grade III: Burns of the dermis, divided into two types:
- Superficial dermis: sweat gland hair follicles are intact, there are skin blisters, wet red background, increased pain sensation, usually recovers after 2-4 weeks
- Deep dermis: only the deep part of the sweat glands, easy to use hair clippers, white spots, pink spots, pain relief, recovery usually after 4-6 weeks.
- Grade IV: burns the entire skin layer, if the burn lesion is less than 5 cm in diameter, it is likely to heal on its own. Larger cases, the possibility of surgery because there is much skin necrosis.
- Wet necrosis: usually burns below 60oC, the skin is white, red-gray, the flowers feel wet, soft, rougher than normal skin, pain is lost, damaged skin often disintegrates or falls off gradually from the 2nd week. .
- Dry necrosis: burn temperature above 60oC, skin is dry, black or yellowish, concave compared to healthy skin, hard to the touch, rough, surrounded by red wrinkles, not disintegrating.
- Grade V: burns to the entire skin. Invasion of subcutaneous tissue, muscle fascia, tendons, bones, joints, blood vessels, nerves, internal organs.
Note: Superficial burns are first, second, and third degree burns. Deep burns are fourth- and fifth-degree burns.
Subclinical
Diagnostic tests that determine the depth of the burn injury are usually available in a specialized hospital.
- Intravenous pigment (methylene blue)
- Intravenous fluorescence (cholorotetracycline)
- Radioisotope (phospho32).
The basic tests evaluate the general state of liver, kidney, heart and lung function of the patient and are the basis for comparing the results of the next review after the patient's systemic disorder caused by the burn injury.
- Record burn diagnosis: burn area, burn depth (at examination), burn location, cause of burns, diagnosis can be changed depending on the time of examination.
- Burn shock:
- Bonus occurs early, when burn area 10% can occur
- Skin burns accompanied by respiratory burns high shock rate
- Occurs in the elderly and children.
Different from traumatic shock: plasma drainage, hemolysis, prolonged progressive renal dysfunction, no bleeding.
- Frank index: each % superficial burn is 1 unit, each % deep burn is 3 units:
- If < 30 units: burn shock rate # 5%
- If 30 – < 50 units: shock rate # 50%
- If 50 – < 120 units: # shock rate 80 – 90%
- If ≥ 120 units: shock rate 100%.
- Clinically: two types:
- Erectile shock is often early in the first few hours, agitation, high blood pressure, rapid pulse
- Shock usually occurs in the 5th, 6th hour after the burn, if the burn is deep and large, it will appear earlier and progress to be severe. Symptoms of hypotension <90 mmHg, hypothermia, oliguria (<30 mL/g). BUN, increased creatinine, cloudy red urine, nausea, persistent vomiting, electrolyte disturbances.
- Symptoms:
- Perforation and ulceration of the gastrointestinal tract, common at the 36th hour
- Alveolar hemothorax, high mortality, common at 12 hours
- Acute renal failure.
TREATMENT
Rule
- Actively resuscitate the patient, quickly bring the patient to a stable state
- Burn wound care
- Perform surgical removal of necrotic skin if present, possibly several times
- Improve the patient's condition, gradually recover the patient's general condition
- Phẫu thuật ghép da, chuyển skin flap che phủ tổn thương bỏng đã cắt lọc bị khuyết da.
Specific treatment
Fluid resuscitation, electrolytes, antibiotics, pain relief, burn wound care, necrosis removal, skin grafting or skin flap transfer.
Recipe Parland
- The first 24 hours use Ringer's lactate solution according to the formula 4 mL kg body weight burn area (first 8 hours of infusion of 1/2 of the total volume, 16 hours of infusion of 1/2 of the remaining fluid).
- 24 hours after Colloid solution 0.5 mL kg body weight burn area and glucose solution 5% 2 liters.
Rodin LB . Formula
- Mild to moderate shock: 3 liters of fluid in the first 24 hours, 2 liters after 24 hours
- Severe, very severe shock: 4.5 liters in the first 24 hours, 3 liters after 24 hours, and 1.5 liters after 24 hours. The composition of infusion solution 1/2 is colloidal solution, 1/4 is saline solution, and 1/4 is other fluid.
- To assess fluid and electrolyte replacement, urine flow monitoring should be maintained at 0.5 mL – 1 mL/kg/hour, and monitor consciousness, pulse, and blood pressure.
- Systemic pain relief infusion of Perfagan, Morphine, ...
- Combination antibiotic, broad spectrum
- Support the general condition, early feeding, parenteral nutrition, through the stomach, ...
Monitor
- Burn wound care: tamanu oil, silver nitrate oiment, Biafine,…
- Physiotherapy
- Psychotherapy
- Necessary surgery.




