Table of contents [hide]
1. OVERVIEW
The human locomotor system consists of bones, cartilage, muscles, tendons, ligaments and soft tissues, divided into two parts: (1) the passive part consisting of the skeleton and the system associated with bones (joints), ( 2) the motor part consists of tendons and muscles, the activity depends entirely on the nervous system. The bones consist of 206 different lengths, which combine to form a skeleton that supports the body and protects organs from injury. The muscular system consists of about 600 muscles, which attach to the ends of bones to help the body move. Thanks to the motor system, our body has a certain shape, we can perform labor movements, and we can express our emotions.
In the locomotor system, bones are linked to each other and to muscle fibers through connective tissues such as tendons and ligaments. Bones provide stability in the body, while muscles help stabilize bones and play an important role in bone movement. The bones are connected by joints and at the ends of the bones there is cartilage to limit friction.
2. SOCIAL SYSTEM PAIN
-
- Reason
The causes of musculoskeletal pain are diverse, can be acute or chronic, can be local or widespread. Caused by trauma such as sudden movements, car accidents, falls, fracture sprains, dislocation and direct impacts on the muscles, etc. can also cause musculoskeletal pain. Other causes include pain from constant tension, repetitive movements, overuse and motionless lengthen. In extreme cases, changes in posture or physical inactivity can cause spinal problems and shorten muscles, causing other muscles to strain and cause pain. Pain from overstretching affects 33% adults, common in low back pain.
Musculoskeletal pain also depends on many factors of the patient such as: age, gender, body shape, activity level and lifestyle.
- Diagnosis and symptoms
Diagnose Motor system pain should be based on:
- Origin of pain: local or penetrating pain, reflex pain (Zakharin Head) or psychological
- Pain may be present in one or more different locations – Factors that reduce or increase pain: changes in posture, movement – Other symptoms (eg, rash, fever, dry eyes, etc.) ).
Symptoms depend on pain caused by trauma or abuse, whether acute or chronic. These symptoms can also vary from person to person.
Symptoms often vary in patients, but are usually:
- Local or extensive pain that changes with movement
- Feeling of muscle being overstretched
- Pain or stiffness in the whole body
- Tired
- Sleep disorders
- Muscle twitching
- The feeling of "burning, burning".
- Classification of types of motor pain
Bone pain: Often felt as deep, sharp, dull pain, often the result of trauma, it is important to ensure that the pain is not related to a fracture or tumor. Other causes include infectious bone pain (myelitis bone), endocrine disorders.
Synovial bag: thường đau tăng khi vận động túi hoạt dịch và giảm khi nghỉ, túi hoạt dịch bị ảnh hưởng có thể sưng lên, gây ra bởi chấn thương, lạm dụng, bệnh gout hay nhiễm trùng.
Muscle pain: Less intense than bone pain but can be very uncomfortable, the pain may include muscle spasms or cramps (eg, a spasm of the calf muscle that causes severe pain commonly referred to as a Charley horse). Myalgia can be caused by trauma, autoimmune reactions, decreased muscle perfusion, infections, or tumors.
Tendon and ligament pain: đau ít hơn đau xương, đau tăng khi các khu vực bị ảnh hưởng bị kéo căng hay di chuyển và luôn giảm khi nghỉ. Nguyên nhân phổ biến của đau gân là viêm gân, viêm bao gân, viêm lồi cầu ngoài hay trong, tổn thương. Nguyên nhân phổ biến của đau dây chằng là chấn thương (bong gân).
Athritis: Joint injuries and diseases always cause stiffness, pain, arthritis. The pain ranges from mild to severe, increases with joint movement, joints may swell. Pain may be acute (eg, infection, trauma, or gout) or chronic (eg, when caused by rheumatoid arthritis or inflammation of the bone joint). Arthritis is a common cause of pain, and arthritis pain is present even at rest. Disorders that can cause arthritis include rheumatoid arthritis, osteoarthritis, septic arthritis, gout and related disorders, autoimmune, and inflammatory vasculitis (such as systemic lupus erythematosus and systemic lupus erythematosus and vasculitis). Schönlein-Henoch allergic vasculitis), caseation bone, an injury that affects a part of the bone inside a joint.
Tunnel syndrome: This disorder causes pain from nerve compression, pain that radiates to the nerve and may feel like a burning sensation, often accompanied by tingling, numbness, or both. Includes: syndrome carpal tunnel, cylindrosis syndrome and tarsal tunnel syndrome.
3. SOME FREQUENT POSITIONS OF PAIN
3.1. Hip pain
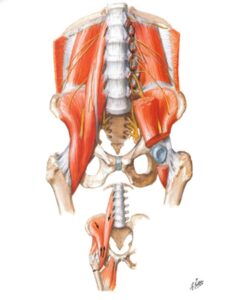
Inside hip joint There is always a minimal amount of fluid that allows the femoral head to rotate within the acetabulum. Any disease or injury that causes inflammation causes this space to fill with fluid or blood, straining the joint capsule and leading to pain.
The femoral head and acetabulum are lined with articular cartilage, allowing the bones to move within the joint with little friction. The acetabulum margin is covered with marginal cartilage, which can be torn or torn, causing pain.
There are thick bands of tissue that surround the hip joint, forming a tight capsule. This helps stabilize the hip joint, especially during movement.
The movement of the hip is due to the surrounding muscles and their tendons attaching across the hip joint. The muscles also help maintain joint stability.
The large fluid-filled sacs that surround the hip joint allow the tendons to slide more easily over the bony ridges. These structures can become inflamed.
Symptoms: Depending on the cause and condition causing the pain, the patient will experience discomfort in:
- Femoral
- In the hip joint
- Inguinal, outside the hip – Buttock area.
Pain increases with activity (especially in the presence of arthritis) and decreases range of motion. Some patients limp if the pain is persistent.
Đôi khi đau từ các khu vực khác có thể lan xuống hông: viêm dây thần kinh tọa (đặc biệt nếu rễ L1, L2 có liên quan), các viêm dây thần kinh có thể biểu hiện như đau hông, thần kinh bì đùi ngoài (thường viêm trong thời kỳ mang thai, mặc quần áo chật hoặc đái tháo đường).
Pain from an inguinal or thigh hernia can also cause pain to be felt in the hip.

3.2.1. Reason
Arthritis: Inflammation in the body can affect the hip joint. Synovitis, or stromal inflammation, causes fluid to leak into the joint, resulting in painful swelling. Osteoarthritis It is a common cause of hip pain in people over the age of 50. Other diseases: arthritis rheumatoid arthritis, ankylosing spondylitis, arthritis associated with inflammatory bowel disease (Crohn's disease or ulcerative colitis). Common symptoms: pain in the groin or front of the thigh, the patient may feel groggy, stiff, or reduced mobility, usually pain immediately and does not get better with activity. Pain develops after a period of inactivity and eases when "warmed up" with use. But as activity increases, the pain returns.
Injury: Usually the cause of hip pain, felt immediately, is more common in the elderly, has osteoporosis causing fractures of the upper femur, acetabulum, pelvic branch or hip dislocation. Cases of contusions (bruises), sprains, strains that can be the result of trauma but not fractures can be very painful, requiring further laboratory tests for diagnosis such as: X-ray, CT scan, MRI.
Tendonitis: Iliotibial band syndrome (ITBS) is common in sports activities, walking, biking, climbing, etc. pain is located on the outside of the pelvis. knee joint, to varying degrees. Pain is relieved at rest, while walking, when performing sports that require a change in the level of running. A steady, continuous, prolonged walk causes pain on the outside of the knee, sometimes causing the patient to stop.
- Piriformis syndrome: a neuromuscular disorder caused by the pear-shaped muscle compressing the sciatic nerve (sitting or running long distances, kicking), the pear-shaped muscle helps to fix the hip joint, lift and rotate the thigh. allow walking, lifting in body weight from foot to foot, maintaining balance. Symptoms usually begin with pain, tingling, or numbness in the buttocks, pain that may radiate down the sciatic nerve, pain when walking up stairs or leaning, increased with prolonged sitting, and decreased range of motion in the hip.
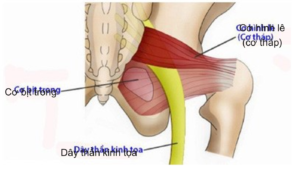
- FAIR test (hip flexion, adduction, internal rotation): the patient was lying on the painless side, the leg was painful at 60° hip flexion, knee flexion, hip adduction, and internal rotation. The examiner applies pressure to the knee in a downward direction, thereby straining the pear muscle and increasing pressure on the sciatic nerve.

- Gluteus medius syndrome: Pain and inflammation in the outer part of the groin caused by a tendon tear (tension) of the gluteus medius muscle. The gluteus medius muscle plays a role in helping to shape the thigh and stabilize the groin when walking, running, and jumping. Consists of two groups: group 1 stretches but does not stretch tendons; group 2: tension and elongation of tendon or partial tear, causing reduced function. Common symptoms: pain, often limping, when walking and running, soft pressure on the outside of the groin. Pain, stiffness, swelling, heat, redness on the outside of the thigh, worse when moving the groin, often with groin weakness, and increasing or weak pain when flexing the thigh.
- Iliopsoas tendinitis and Iliopsoas syndrome: tendinitis caused by repetitive flexion of the groin or overuse of the groin, iliopsoas syndrome caused by sudden contraction of the muscle, resulting in muscle tearing, Common in athletes who run, jump, and sports that require kicking or lifting weights. Common symptoms: pain in the groin, thighs when walking or running, with back pain; Flexion of the hip joint is weak and painful, reducing the force, in some cases can be stiff. Examine this case for the patient to lie down, bend the knee 10 - 20o, raising the leg is antagonistic, pain occurs with lumbosacral fasciitis.
Injury to joint capsule, cartilage, border cartilage: Often due to overuse, pain begins minutes or hours after the injury, then causes muscle spasms and the joint surface becomes inflamed, causing fluid accumulation. Pain is usually anterior to the groin, but may be outside the groin or buttocks area, and may lead to a limp.
Synovitis: The bursae around the trochanter are often inflamed from trauma or overuse.
Other causes:
- Due to inguinal or thigh hernia?
- Gynecological or back: when the lining of the uterus grows or pain due to damage from the nerve roots
- Sickle cell disease: a joint may swell during an active episode with or without an underlying infection. The hip is not the only joint affected
- Viral or bacterial infections: Lyme disease, Reiter's syndrome and food poisoning infections
- Avascular necrosis of the femoral head: may occur in long-term corticosteroid users. The femoral head loses its blood supply, causing gradual necrosis and pain
- Legg-Perthes-calf disease (or Perthes disease) describes avascular necrosis of the femoral head in children and is idiopathic, meaning the etiology is unknown. It usually affects men between the ages of 4 and 8
- Fibromyalgia: systemic pain syndrome associated with pain and stiffness.
- Bone cancer.
3.2.2. Conclude
Hip pain is a non-specific complaint that requires a healthcare professional to find the underlying cause of potential injury or illness. Approaching the diagnosis of hip pain requires an open mind, because the source of the injury or the cause of the disease is unclear. 3.3. Knee pain
3.3.1. Anatomy
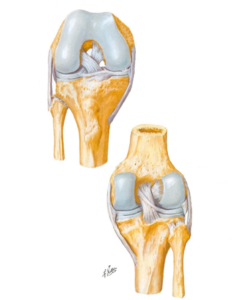
The main function of the knee joint is flexion, extension and movement, partly twisting and turning. The structure includes:
- Bones: femoral condyle, tibial plateau, patella, fibula cap
- Ligaments: there are 4 ligaments in the knee joint including cruciate ligament anterior (ACL), ligament rear cross (PCL), lateral ligament medial (MCL), external ligament (LCL)
- The patellar muscle and tendon are two important structures
- articular cartilage and meniscus: create space and cushion for the knee joint
- Synovial sacs: there are four important groups of synovial sacs: below the quadriceps tendon, below the patella, below the patellar tendon, and the gooseberry muscle (inside and below the knee joint 3 cm).
3.3.2. Reason
Fracture: Often due to high impact injuries, severe pain is felt and the patient is unable to put pressure on the knee. X-ray is a simple and highly effective measure.
Ligament damage:
- Tổn thương ACL là tổn thương hay gặp nhất, thường gặp trong sports injury
- PCL is stronger than ACL and is less likely to be torn, common in traffic injuries, often with other ligament damage and fractures
- The MCL is most often affected and the LCL is rarely affected
- When the ligaments are injured, the patient may hear a "pop" sound, pain that feels like a tear or split, and instability of the knee. Examination: drawer test, closed form, Lachmann... MRI of knee joint or endoscopy for diagnosis.
Meniscus damage: may be due to injury or excessive movement of the knee, the knee may be locked in a position or hear a "click" sound when moving and rarely swollen. Examination: Apply test, Mc Murray… MRI of knee joint or endoscopic examination for diagnosis.
Knee dislocation: This is a rare injury and an emergency. Knee dislocation can be accompanied by damage to arteries, nerves, the knee will be clearly deformed and if it is not completely dislocated, there may be a "clump" sound. It is necessary to take X-ray, MRI for diagnosis and Doppler ultrasound of blood vessels to investigate whether there is associated vascular injury or not.
Tea cakes: thường do chấn thương trực tiếp hoặc duỗi mạnh, phổ biến gặp ở phụ nữ người béo phì, chân chữ O và người có xương bánh chè nằm cao. Bánh chè có thể trật sang hai bên, khó khăn khi gập, duỗi gối. Chụp X-quang ở tư thế mặt trời mọc, chụp MRI để phát hiện trật bánh chè và các tổn thương đi kèm.
Arthritis:
- Osteoarthritis: due to degeneration of knee cartilage, meniscus is worn down, the lower end of the femur will rub against the top of the tibia (bone touching bone). Symptoms: persistent pain, increased with movement, the knee joint may be stiff when sitting for a long time.
- Rheumatoid arthritis: is a systemic disease affecting many joints. Symptoms: knee pain and stiffness in the morning, there is pain in other joints, the knee may be warm and swollen. X-rays and blood tests for diagnosis.
- Crystal inflammation (gout and pseudogout): caused by crystals forming in the knees and joints: urate (gout), calcium pyrophosphate (pseudogout). Symptoms: rapid onset, marked inflammation, decreased mobility. X-rays, blood tests, or joint fluid tests to make a diagnosis.
- Synovitis: due to trauma, infection, crystal deposition. Symptoms: acute trauma with pain and swelling due to bursitis. The most common bursitis is anterior patellar bursitis (usually in housekeepers, or carpeters) and secondarily goose bursitis (common in obese women, athletes): Pain increases with folding of the pillow or at night while sleeping.
- Infection (septic arthritis): many bacteria can spread to the knee: gonorrhea or bacteria that stay on the skin or due to decreased resistance. Symptoms: local or systemic infection (fever, chills).
- Other causes: patellar femoris syndrome and patellar luxation (Patellofemoral syndrome and chondromalacia patella), Osgood-Schlatter disease, jumper's knee (Jumper's knee), iliotibial band inflammation, etc.
3.3.3. Subclinical
- X-rays and CT scans show fractures, dislocations, joint spaces, and joint changes
- MRI scan: survey of ligaments, tendons and cartilage
- Joint fluid test
- Blood tests: infection, rheumatoid arthritis and diabetes.
3.4. Pain in ankles and feet
3.4.1. overview
The ankle-foot joint is a combination of the bones of the lower leg and foot, and pain in this area can be caused by inflammation or injury. There are about 20 muscles involved in neck-foot activity, with the main muscles: tibialis anterior, posterior tibialis, fibula, flexor, extensor, and the strongest tendon is the Achilles tendon.
3.4.2. Anatomy
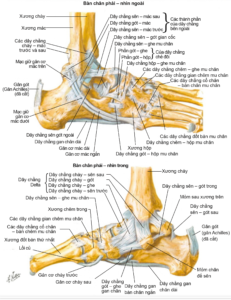
- Ligaments: The longest is the plantar fascia, the internal and external ligaments help stabilize the ankle.
- Synovial bag:
+ Ankle: synovial sac behind the heel, under the skin of the heel, under the skin of the inner ankle
+ Feet: synovial sac of metatarsal bone, metatarsal joint - toe I, calcaneus.
3.4.3. Reason
Achilles tendon pain (heel tendon): May be due to tendinitis or tendon rupture.
Tendonitis: is a common disease, especially common in athletes or patients who have to walk a lot. Pain is usually at the bottom of the tendon where the tendon attaches to the heel bone.
Tendon rupture: partial or complete, occurs when the tendon is stretched beyond its capacity. Most commonly seen in cases of “weekend warrior syndrome” (middle-aged people participating in sports in their spare time). It can be caused by illness or by taking steroids or antibiotics that can cause tendons to tear easily. Examination: evaluate bilateral range of motion and muscle strength, difficulty standing on toes, do Thompson's test.
Tendon injury: The fibula helps stabilize the foot and ankle, helping to prevent sprains, often in athletes with repetitive ankle movements or those with high arched feet.
Posterior tibial tendon: condition that impairs tendon function, causing weakening of the arches of the feet and flat feet. Also known as “adults with flat feet”. Cause: overuse (such as running, walking, hiking, or climbing stairs).
Injury to the talus arch: due to trauma causing defects or damage to the talus cartilage. Symptoms: deep chronic pain at rest, increasing with load on the ankle, feeling of stalling or jamming when walking, feeling in the back of the ankle that locks or pops, swelling on load and decreases with rest.
Carpal tunnel syndrome: The tarsal canal is a narrow space inside the ankle in which the posterior tibial nerve is encountered when the nerve is compressed. Patients are at high risk for: flat feet, tube abnormalities (varicose veins, cysts, lymphadenopathy, tendon swelling and arthritis), diabetes.
Plantar Tendonitis or Achilles Tendonitis: due to wearing high heels, gaining weight, walking, standing or climbing stairs a lot, abnormal foot arch. Symptoms: heel pain when walking, standing and even at rest, pain occurs in the morning before getting out of bed.
Other causes: Gout or degenerative arthritis, sprains, fractures, diabetic neuropathy, Raynaud's syndrome, bursitis, etc.
3.4.4. Subclinical
- Blood tests:
+ Erythrocyte sedimentation (ESR), C-reactive protein (CRP), white blood cells
Rheumatoid arthritis: rheumatoid factor
Systemic lupus erythematosus: antinuclear antibodies
Lyme disease: antibodies to the bacteria that cause the disease
+ Gout: uric acid...
- Urine test
- Joint fluid testing: urate crystals, bacteria, etc.
- X-ray: suspected fracture, bone tumor or infection, or a change in arthritis (rheumatoid arthritis or osteoarthritis)
- MRI: suspect ligament and tendon damage or damage to important structures in the joint; It may not be better than a standard X-ray in the evaluation of many types of pain. MRI can detect fractures that don't show up on X-rays
- CT scan: gives a better picture than X-rays of bone problems
- Contrast-enhanced imaging: eg, intra-articular injection to examine structures such as ligaments
- Bone scan.




